

Grace Fox, MPP, Tribal Healthcare Policy Analyst, Native Nations Center for Tribal Policy Research
Purchased/Referred Care (PRC) is a program of the Indian Health Service (IHS), located in the U.S. Department of Health and Human Services. Tribal citizens, or members of federally recognized Indian tribes, may receive healthcare services from an IHS or tribal healthcare facility. When services patients need are not available or accessible at IHS or tribal healthcare facilities, the PRC program authorizes and pays for eligible healthcare from providers that are not IHS or tribal providers.
This report describes how PRC is structured and administered and describes its rules, workflows, and funding. This report first outlines core program elements—eligibility and PRC Delivery Areas (PRCDAs); notification and documentation timelines; medical-priority levels; alternate-resource coordination; staffing and claims processes; and funding constraints. It also summarizes key findings from federal audits, tribal Congressional testimony, and recent policy initiatives related to PRC administration.
This report emphasizes the PRC process as it relates to cancer care. Cancer is an increasingly important public health priority in Indian Country. As described in this report, American Indian and Alaska Native (AI/AN) populations experience later-stage diagnoses, lower screening participation, and higher mortality than the U.S. population overall. Further, cancer incidence—or the rate of newly diagnosed cancer cases—exceeds that of other populations for lung, colorectal, and kidney cancers. These patterns underscore the importance of timely access to cancer care for AI/ANs.
As this report describes, tribal citizens may seek cancer care from various providers. One way is through the PRC program. In the cancer context, PRC supports oncology diagnostics and treatment, and the timing of PRC authorization and processing can directly affect how quickly abnormal screens move to diagnosis and treatment for tribal citizens. Specifically, this report examines how PRC intersects with cancer screening, diagnosis, treatment, and follow-up. The analysis then links these structural features to specific points along the cancer care pathway where delays or gaps are most likely to occur, with attention to national and Oklahoma-specific cancer data for AI/AN populations. Because many of these services are delivered by non-IHS/tribal providers, PRC often functions as the authorizing and paying mechanism when local specialty capacity is unavailable or not accessible in a timely way.
Tribal decision-makers may consider several policy options for addressing the PRC process with an emphasis on cancer care pathways. The options are organized around tribally led, sovereignty-driven strategies grouped into six thematic areas, including: 1) self-determination and self-governance under the Indian Self-Determination and Education Assistance Act; 2) coverage and financial protection, including approaches that expand enrollment in Medicaid, Medicare, marketplace plans, and private group coverage; 3) regional collaborations and partnerships, in which intertribal consortia, academic centers, and national nonprofits pool demand and centralize; 4) service-delivery models, such as mobile screening, shared satellite clinics, and teleoncology, that allow components of cancer care to be more accessible; 5) care coordination, navigation, education, and communication that support timely completion of referred-care steps; and 6) sovereignty-driven federal engagement, in which tribes may use budget formulation, consultation, workgroups, congressional testimony, and coalition advocacy to shape federal decisions about IHS and PRC policy.
For tribal citizens, many steps in cancer care—diagnostic imaging, biopsy and pathology, staging studies, radiation therapy, and subspecialty visits—are often delivered by providers that are not in the Indian Health Service (IHS) and are not tribal providers. If tribal citizens, defined as citizens or members of a federally recognized Indian tribe (tribe or Tribal Nation), receive healthcare from IHS or tribal facilities, they may be referred to non-IHS/tribal providers, or sometimes referred to in this report as outside providers, when cancer care they need is not available.[1] Access to these referred oncology services is managed through the Purchased/Referred Care (PRC) program.
PRC is the IHS program, located in the U.S. Department of Health and Human Services (HHS), that purchases eligible care from outside providers when: 1) no IHS or tribal direct care facility exists; 2) an IHS or tribal facility cannot provide the required emergency and/or specialty care; 3) a facility’s capacity is exceeded; or 4) supplementing alternate resources is necessary for comprehensive care.[2] PRC functions as a bridge between IHS and tribal facilities that provide direct care (health services delivered in-house at an IHS or tribal clinic or hospital) and outside providers in the broader health care system. PRC operates under federal regulations that establish eligibility and medical-priority criteria and, as the payer of last resort, requires the use of other available coverage before PRC funds are applied.
This report describes how PRC functions in practice with emphasis on cancer screening, diagnosis, and treatment. Federal oversight and program rules identify structural features that can affect whether and how quickly patients can obtain referred services at different points in their cancer care. PRC eligibility and administrative requirements—including residency rules tied to a tribe’s designated PRC Delivery Area (PRCDA), medical-priority categories, alternate-resources verification, and documentation/notification timelines—can influence the timeliness of access to specific services (e.g., scheduling cancer screenings or initial oncology visits). These requirements may also affect approval or payment for referred services (e.g., ineligibility due to residence outside a PRCDA, or denial pending proof of other coverage).
Tribal Nations may choose to respond to PRC-related cancer challenges through multiple, interconnected strategies. This report first describes how PRC is structured and administered, then summarizes federal oversight findings and recent policy developments, and reviews cancer burden data for American Indian and Alaska Native (AI/AN) populations with emphasis on Oklahoma. It then presents tribally focused policy options for consideration, grouped into the following thematic areas: 1) self-determination and self-governance; 2) coverage and financial protection; 3) regional collaborations and partnerships; 4) service-delivery models that bring oncology care closer to patients; 5) care coordination, navigation, and education; and 6) sovereignty-driven federal engagement on IHS and PRC policy.
For the purposes of this report, the below terms are defined and are generally applicable throughout this report. Other terms may defined for specific purposes throughout the report as well.
Direct Care – Direct care refers to medical and dental services provided through direct patient–provider interaction, which occurs on-site at either IHS or tribal health facilities. This differs from Purchased/Referred Care, which supports eligible care delivered by outside providers through referrals and is subject to eligibility rules and funding availability.
IHS Direct Service – IHS direct service refers to care delivered to tribes through federally operated IHS facilities and service units. This differs from tribal health clinics, which are facilities operated by tribes under Indian Self-Determination and Education Assistance Act agreements using IHS funding. Both provide direct care to eligible AI/ANs and, when needed services are not available locally, may initiate referrals for PRC-supported outside care.
PRC Referral (Provider Referral) – A PRC referral (used interchangeably in this report with provider referral) is the clinical request initiated by an IHS or tribal clinician (or clinic staff on the clinician’s behalf) to obtain medical or dental care outside the IHS/tribal facility because the needed service is unavailable locally or capacity is exceeded. A referral starts PRC review but does not guarantee PRC payment.
PRC Application – A PRC application is the patient-facing eligibility and documentation process used by some programs to establish or confirm baseline eligibility for PRC (e.g., PRCDA residency, tribal citizenship or descent documentation, and alternate-resource coverage). Not all programs use the term “application” formally; in many settings, it refers to the packet of forms and supporting documents PRC staff require to confirm eligibility and process a request.
PRC Approval – PRC approval is the decision by the PRC program/ordering official that a specific requested service meets PRC requirements (including eligibility, medical necessity, medical priority/funding availability, payer-of-last-resort/alternate resources, and notification/timeliness rules). PRC approval generally means PRC is prepared to authorize the service for potential payment, subject to scope and conditions.
PRC Purchase Order or Authorization – A PRC purchase order is the formal authorization instrument issued by PRC that specifies what is approved for outside care—typically including the patient, provider/facility, authorized services, dates or units/visits, and any limits or conditions. In practice, “authorization” and “purchase order” are often used together because the purchase order documents and tracks the authorization. This report uses purchase order, PRC authorization, or authorization interchangeably.
PRC Payment/Reimbursement – PRC payment/reimbursement is the payment made to the outside provider (or fiscal intermediary) after care is delivered and a claim is submitted. Payment occurs only if the claim matches the purchase order/authorized scope and all conditions are satisfied (including alternate resources billed first and required documentation/notification on file). PRC approval and authorization do not guarantee reimbursement if later conditions are not met.
The federal trust responsibility to provide health care to AI/AN people arises from treaties, statutes, and the government-to-government relationship between tribes and the United States. Through foundational laws, such as the Snyder Act of 1921, Congress began establishing health services for AI/AN people.[3] In 1954, Congress transferred health functions from the Bureau of Indian Affairs (BIA) in the U.S. Department of the Interior (DOI) to the U.S. Public Health Service.[4] In 1955, Congress created the Indian Health Service (IHS), within the U.S. Public Health Service (now within HHS), and began operationalizing the federal government’s trust responsibility for AI/AN health care.[5] In 1976, Congress reaffirmed this responsibility in the Indian Health Care Improvement Act (IHCIA).[6]
In practice, this federal trust responsibility was often carried out through IHS direct service facilities, which are federal medical facilities that provide direct care to tribal citizens. Direct care refers to medical and dental services provided on-site at IHS or tribal health facilities, involving direct patient-provider interaction within the facility.[7] However, direct care facilities were not always equipped to meet the full range of patient needs. For complex or high-cost conditions, patients often needed to seek care beyond IHS and tribal facilities, making referred care a necessary part of the system.
The IHCIA formally created and authorized Contract Health Services (CHS) to purchase care from non-IHS/tribal providers when specialty direct care services were not available at IHS or tribal facilities, capacity was exceeded, or comprehensive care required supplementation of alternate resources.[8] In 2014, Congress changed the program name from CHS to Purchased/Referred Care (PRC) to reflect both the purchase of outside services and the referral processes that precede payment.[9]
PRC therefore sits at the intersection of IHS direct service facilities or tribal medical systems and the general U.S. health care network, with eligibility and priority rules established in statute and regulation. PRC eligibility and priority rules will be discussed in more detail in the “PRC Eligibility” section of this report. Next, this report discusses PRC administration in IHS direct service facilities and under the Indian Self-Determination and Education Assistance Act authorities as each intersect with the PRC program.
PRC is administered under uniform federal requirements, primarily the IHS regulations at 42 CFR Part 136, which establish general principles and requirements for carrying out Indian health programs.[10] However, day-to-day operations differ depending on whether services are delivered by an IHS direct service facility or by a tribal health program operating under the Indian Self-Determination and Education Assistance Act (ISDEAA), discussed in more detail below.
As noted above, in IHS direct service settings, the IHS is responsible for providing health care services directly to Tribal Nations and their citizens. PRC functions are typically performed by staff at IHS Area offices (regional administrative units) and IHS Service Units (local IHS facilities or facility networks). These staff screen referrals for unavailable specialty care initiated by an IHS or tribal provider against program rules, including verification of PRC eligibility, assignment of a medical-priority level, and review of medical necessity. It also includes confirmation that alternate resources have been used first because PRC is the payer of last resort. Based on this review, PRC staff issue authorizations to outside providers or, when criteria are not met, defer or deny payment.[11]
For many Tribal Nations, self-determination and self-governance of health services is a pathway to align care delivery with their community priorities, diversify revenue, and reduce dependence on PRC processes. Congress enacted ISDEAA in 1975.[12] As enacted, ISDEAA authorized DOI and the Department of Health, Education, and Welfare (now the HHS) to enter into self-determination contracts, sometimes referred to as 638-contracts, with tribal governments so that tribes could operate programs and services for AI/AN people that had previously been administered by the BIA and the IHS.[13] Subsequent amendments in 1992 authorized a Tribal Self-Governance Demonstration Project within IHS, giving participating tribes the option to enter self-governance compacts for specified health programs.[14] In 2000, Congress enacted the Tribal Self-Governance Amendments (P.L. 106-260),[15] which created Title V of ISDEAA and established a permanent statutory framework for the IHS Tribal Self-Governance Program.[16]
Under ISDEAA Title I self-determination contracts and Title V self-governance compacts, tribes may assume responsibility for health care operations historically run by IHS. Briefly, compacts generally provide greater flexibility than contracts: Title I contracts involve more direct federal oversight of the contracts. Under Title V compacts, tribes may redesign or consolidate programs, services, functions, and activities and reallocate or redirect associated funding without prior IHS approval, subject to ISDEAA and other applicable federal law.[17] In all cases, tribal programs operated under ISDEAA remain bound by the statute, implementing regulations, and the terms of their funding agreements.[18]
Under these same authorities, tribes may elect to assume administration of the PRC program. When a tribe includes PRC among the programs, services, functions, and activities in its ISDEAA self-determination contract or self-governance compact, the PRC funds that would otherwise be managed by IHS are added to the tribe’s funding agreement. The tribe then administers PRC under its own federally approved PRC policies and procedures, consistent with federal law and regulation.[19] Tribal governments may, but are not required to, supplement these federal PRC funds with tribal dollars. For example, tribal dollars may be used to expand eligibility, pay for services that fall outside PRC medical-priority levels, or address shortfalls near the end of the funding cycle. Tribes may also use third-party revenues (such as Medicaid, Medicare, and private insurance collections) to support referred care, consistent with their own financial policies.
Under ISDEAA Title I self-determination contracts, tribes may administer PRC but generally do so under the terms of the contract and applicable federal requirements. Title I contracts typically allow less flexibility to redesign program operations or reallocate PRC-related funds without IHS approval.
Under ISDEAA Title V self-governance compacts, tribes have more flexibility to operate their PRC programs. Tribes may manage referral review, authorizations, vendor relations, and claims/payment workflows. They also may tailor operations—such as navigation support, timelines, and memoranda of understanding with local providers—to meet tribally specific conditions.
In both IHS direct service and ISDEAA models, PRC funding is part of the IHS budget that is allocated to IHS Areas and to tribal programs. Specific eligibility requirements must be met by each person needing and applying for PRC assistance.[20] These conditions are discussed in more detail in the next section of this report, “PRC Eligibility.”
PRC eligibility criteria define who can receive PRC assistance. This section first provides an overview of baseline eligibility for IHS services and residence within a PRC Delivery Area (PRCDA). Second, this section reviews authorization conditions that apply to each specific episode of care, including requirements related to timely notification and documentation, funding availability, and medical priority. PRC payment depends on meeting both baseline eligibility and these authorization conditions at the time of referral.
Importantly, PRC is not an entitlement program; in other words, an eligible individual does not have a guaranteed right to PRC payment for any particular service. Authorization of payment is contingent on the following:
· availability of funds;
· compliance with alternate-resource rules; and
· satisfaction of all documentation and notification requirements.
As a result, coverage is not automatic. Denials or deferrals can occur when a patient resides outside the PRCDA, when alternate resources must be used first, when required timelines or documents are not met, or when requested services do not meet applicable medical-priority criteria. PRC referrals are discussed in more detail in the section titled, “PRC Referral Management.”
Baseline eligibility for PRC rests on two foundational elements: citizenship/descent and geography. Citizenship/descent criteria determine whether an individual is eligible for IHS services as an American Indian or Alaska Native (AI/AN) or as another eligible person under federal law. Geography-based criteria determine whether that individual resides within a PRCDA associated with a particular IHS or tribal health program. The subsections below describe how these citizenship/descent and geography requirements operate together to establish baseline eligibility before visit-specific authorization conditions are applied.
PRC eligibility generally begins with eligibility for IHS direct care, with limited exceptions.[21] An individual typically must be able to establish eligibility for IHS services—most commonly through documentation of citizenship in a federally recognized tribe or descent from an enrolled citizen—and this requirement applies whether direct care is provided in an IHS direct service setting or through tribally operated facilities under ISDEAA. Meeting this citizenship/descent baseline eligibility is necessary for PRC referral authorization but not sufficient alone; payment for a specific episode of care also depends on meeting the additional authorization conditions described throughout this section.
Under 42 CFR § 136.12, an individual must provide proof of enrolled membership in a federally recognized tribe or proof that they descend from an enrolled member of a federally recognized tribe.[22] As of December 18, 2025, the federal government recognized 575 federally recognized Indian tribes, acknowledged either through an Act of Congress or through the Department of the Interior’s administrative acknowledgment process.[23] Documentation of tribal citizenship or descent is required and is reviewed by the local IHS Service Unit (the IHS facility or network that serves the patient’s community) or by the relevant tribal health program as part of eligibility determination for both IHS direct care and PRC.
PRC coverage may also extend, in limited circumstances, to a non-Indian (i.e., not a member of a tribe) woman pregnant with an eligible Indian’s child (through six weeks postpartum), certain non-Indian household members in a public-health hazard, and adopted, foster, or stepchildren up to age 19.[24] When these special-circumstance categories apply and required documentation is provided, individuals may be treated as eligible for PRC on the same basis as other eligible persons, subject to compliance with all PRC rules and the same funding, medical-priority, and authorization conditions described elsewhere in this report.[25]
Under 42 CFR § 136.23, PRC residency generally requires that an eligible person live on a reservation or, if not on a reservation, within a PRCDA. In most regions, a PRCDA consists of one or more counties that include all or part of a reservation and additional adjacent counties that are formally designated for PRC purposes. For PRC, “reservation” includes federally recognized reservations, pueblos, colonies, former reservations in Oklahoma, Alaska Native regions established under the Alaska Native Claims Settlement Act, and Indian allotments, as defined in federal regulation.[26] Figure 1 below provides a national map providing a general overview of the delineation of PRCDA designations across the United States.
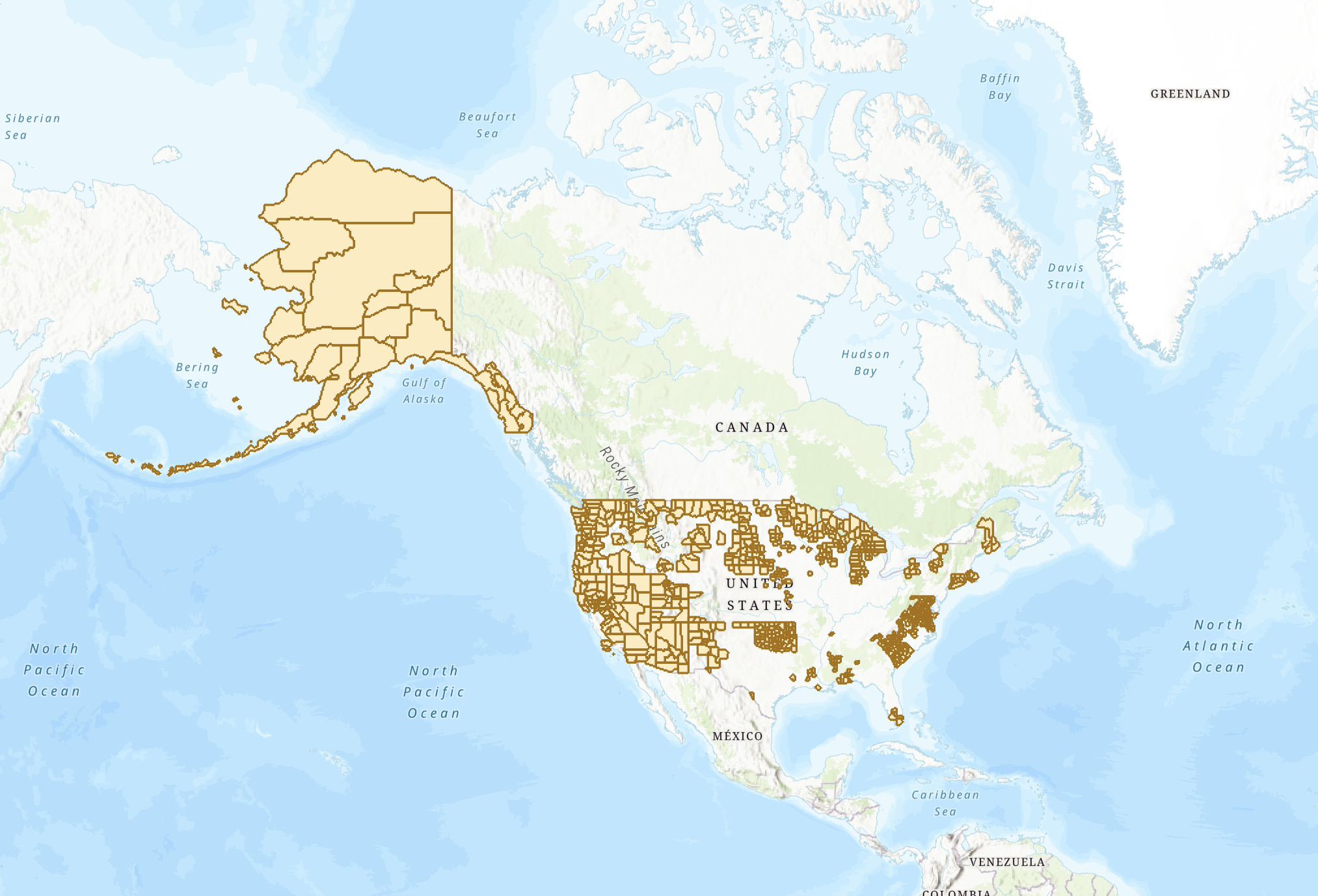
Figure 1. 2023 Purchased/Referred Care Delivery Areas from ArcGIS.com.[27] The map shows PRCDAs across the United States. The darker yellow colors generally depict the external boundaries of the PRCDAs, and the lighter yellow color generally depict the land bases within the external boundaries of the PRCDA. All other colors generally depict land areas outside of PRCDAs and are areas not eligible for PRCDA. This map is for illustrative purposes only. Please contact your local IHS area office for specific information about PRCDAs in your area.
In addition to location, PRC residency also reflects the relationship between the individual and the tribe(s) served by the facility. In general, the individual must either be a member of a tribe located on that reservation or in that PRCDA service area, or be another eligible AI/AN person who resides there and maintains close economic and social ties to that tribe (for example, members of other federally recognizes tribes).[28] These provisions apply to eligible AI/AN individuals and, absent an exception in a limited circumstance discussed above, do not extend PRC eligibility to non-Indians who simply reside in a PRCDA. Residency is defined as “where a person lives and makes his or her home” and is documented by acceptable proof—such as housing, utility, or other records—as determined by the local IHS Service Unit or tribal health program. The individual bears responsibility for providing this documentation.[29]
Living outside PRCDA boundaries generally renders an otherwise-eligible patient ineligible for PRC. The residency requirement therefore has implications for patient eligibility, with few exceptions.[30] Notably, using 2020 U.S. Census data, IHS estimates that approximately 87% of AI/AN people live in urban areas and 13% live on reservations or tribal lands.[31] These figures may provide context to whether or not patients are eligible for care.
In most states, PRCDAs are limited to counties contiguous to a reservation, which may cover significant portions of a state but do not encompass the entire state. As a result, otherwise-eligible citizens who live outside PRCDA counties—including those in metropolitan areas where many IHS-eligible AI/AN people reside—are generally not eligible for PRC. In Oklahoma, all 77 counties are designated PRCDAs, providing statewide PRC residency eligibility under IHS rules and Federal Register notices.[32] Even with this statewide eligibility exception, individuals in Oklahoma must still meet the same referral, medical-priority, funding-availability, and documentation requirements as PRC patients elsewhere. PRCDA boundary designation affects residency only and does not waive other PRC conditions.
These geographic constraints have, in some cases, prompted tribes to request expansion or re-designation of their PRCDA so that more of their citizens can qualify for PRC while living, working, or studying outside existing PRCDA boundaries. Congress has, at times, created or re-designated PRCDAs by statute.[33] The IHS Director may also designate or re-designate PRCDAs administratively to effectuate congressional intent—for example, a 2025 Federal Register notice re-designated the PRCDA for the Chippewa Cree Tribe of the Rocky Boy’s Reservation, Montana.[34] By expanding the PRCDA to include Cascade County in the State of Montana, the Chippewa Cree Tribe’s PRC-eligible population increased by an estimated 251 tribal members.[35]
Authorization conditions apply to each specific episode of care. Authorizations can be either evaluated at the time a referral for care is made or when a claim is submitted for PRC payment. Even when a patient meets baseline PRC eligibility, payment for a particular visit depends on factors such as timeliness of notification; availability of PRC funds; and medical-priority level. The subsections below describe how these factors operate during the PRC referral and authorization process and how they can affect whether PRC can pay for a given episode of care. The “PRC Referral Management” section of this report describes these referral and approval processes in more detail, step by step.
If an individual seeks outside care that may be covered by PRC funds, the patient (or someone acting on the patient’s behalf) and/or the outside facility must notify the appropriate IHS or tribal PRC office within required timeframes. Notification is the mechanism that allows the PRC ordering official to document the episode, confirm whether the situation is emergency or non-emergency, and determine whether a PRC approval and purchase order can be issued for potential payment.[36] Notification requirements differ for emergency and non-emergency care, and whether individuals meet these requirements can affect whether and how services are authorized.
IHS defines “emergency services” as a condition that, without immediate treatment, could reasonably be expected to result in serious jeopardy to health, serious impairment of bodily functions, or serious dysfunction of any bodily organ or part. In practice, emergency care includes visits to the emergency room or trauma center in response to life or limb-threatening injuries.
For emergency care, the individual—or anyone acting on the individual’s behalf—must notify the PRC office within 72 hours after emergency treatment begins or a hospital admission occurs.[37] For elders (age 65 and older) and people with disabilities, the notification window extends to 30 days.[38] Notification is typically made by telephone, in person, or through other contact methods specified by the local PRC office; facilities generally provide contact information and instructions in patient materials and on their websites. The notice should include enough information—such as the patient’s identity, dates and location of care, and reason for the visit—for PRC staff to assess eligibility and document the circumstances of the emergency.[39]
IHS defines “non-emergency services” as all care that does not meet the definition of emergency. In practice, non-emergency care includes planned or routine services such as scheduled specialty visits, diagnostic imaging, elective procedures, or follow-up appointments.
For non-emergency care, PRC requires advance notification to the PRC office and prior approval from the IHS or tribal ordering official before receiving outside services in order for PRC payment to be considered.[40] This advance approval is intended to avoid “self-referrals,” circumstances in which patients obtain outside non-emergency care without a PRC referral and may become personally liable for the cost of those unapproved medical services. In this PRC pathway, the advance notification most often occurs through the provider referral process itself: an IHS or tribal clinician initiates the referral, the PRC office reviews eligibility and other requirements, and—if approved—PRC issues a purchase order/authorization before the outside appointment is scheduled.
Because cancer screening, staging, and treatment are typically delivered through planned services, individuals typically receive PRC care through the non-emergency, provider-referred PRC pathway, which is the predominant PRC process discussed throughout this report.
The PRC program is the payer of last resort. Federal regulations establish IHS (including PRC) as the payer of last resort for eligible services—meaning PRC will not authorize or pay for services to the extent another coverage source is available, would be available upon application, or would be available, but for the individual’s eligibility for IHS/PRC services.[41] When PRC authorizes a service, it indicates that PRC will consider payment consistent with these payer-of-last-resort rules after alternate resources have been billed.
42 C.F.R. § 136.61(c) defines “alternate resources” as health care resources other than those of the IHS.[42] These include other health care providers and facilities, as well as federal programs that pay for health services—such as Medicare Parts A and B and Medicaid under titles XVIII and XIX of the Social Security Act—along with state or local health programs and private insurance.[43]
In practice, IHS Service Units and tribal health programs screen referrals for alternate coverage and may require proof of eligibility, enrollment, or application before issuing PRC authorizations.[44] Before PRC payment is authorized, programs must verify and coordinate other coverage—Medicaid, Medicare, Veterans Health Administration benefits, private insurance, and certain state programs.[45] Acceptable documentation typically includes insurance identification cards or eligibility letters; Medicaid or other program approval notices or application receipts; Medicare entitlement notices; VA coordination records; or formal denial notices when applicable.[46] PRC program representatives may assist individuals with enrollment and coordination steps, but individuals are ultimately responsible for furnishing documentation sufficient to substantiate eligibility or application status.
When alternate coverage exists, benefits are coordinated by PRC staff in collaboration with billing and office personnel. In general, the alternate resource is billed first, and PRC considers any remaining balance consistent with program policy and available funds. When coverage is partial or fragmented, staff may need to determine which services are billable to which payer, what deductibles and coinsurance apply, and whether PRC is able to assist with residual balances. PRC decisions may be deferred or denied pending completion of required applications or verifications; in practice, this means that patients who are eligible for other coverage may not receive PRC authorization until they have applied for, or demonstrated enrollment in, those alternate resources.[47]
For cancer, this alternate-resource requirement can be complex, because oncology care often involves multiple providers, repeated services over many months, and separate authorizations for imaging, surgery, systemic therapy, radiation, and supportive care. Tribes have noted that, for time-sensitive conditions such as cancer, this sequence can introduce delays between the clinical decision to proceed with treatment and the point at which all payers have confirmed their roles. These delays may be experienced as administrative uncertainty, repeated requests for documentation, or difficulty determining what portion of care, if any, PRC can support. This alternate resource requirement is a core part of PRC authorization, influencing both the timing of decisions and whether PRC funds are available for a given episode of care.
When funds are insufficient to meet the volume of PRC need within a PRCDA, authorizations are determined on the basis of relative medical need as described under 42 C.F.R. § 136.23(e).[48] In this context, relative medical need refers to how urgently care is required and the potential consequences of delaying or foregoing treatment. Services that address life-threatening or severely disabling conditions are prioritized ahead of those that are routine, elective, or can safely be deferred.[49]
PRC medical priorities are determined during the referral review process, which is when IHS or tribal PRC staff and clinicians evaluate a request for outside services against program rules and available funding. For non-emergency care initiated through an IHS or tribal referral, this review typically occurs after an IHS or tribal provider submits a referral and before the outside service is scheduled. For emergency care, review and authorization may occur after services are delivered, subject to PRC notification and documentation.
PRC medical priorities are usually assigned by IHS or tribal providers, but some routine referrals may be prioritized and authorized by nurse case managers or other designated PRC staff to expedite processing. Some IHS Service Units also use standing orders—pre-approved protocols that allow designated PRC staff to move specified services forward without a separate case-by-case provider order. For example, routing certain high-priority screening or follow-up services directly for authorization once eligibility and documentation requirements are met.
Effective January 1, 2024, IHS revised the Medical Priority Levels framework with the aim of improving consistency and aligning authorizations across preventive, behavioral health, chronic, and acute care.[50] The 2024 update also commits IHS to a systemwide review and update of Medical Priority Levels at least every four years.[51]
Under this updated policy, PRC services are divided into four general categories, each of which is to be given equal consideration:
A. Preventive and Rehabilitative Services;
B. Medical, Dental, Vision, and Surgical Services;
C. Reproductive & Maternal/Child Health Services; and
D. Behavioral Health Services.[52]
Within each category, services are ranked across three priority levels: Priority 1 (Core/Essential), Priority 2 (Intermediate/Necessary), and Priority 3 (Elective/Justifiable).[53] For more information for how the Medical Priority Levels shapes the cancer pathway, see section titled, “How PRC Shapes the Cancer Care Pathway.”
IHS-operated PRC programs are expected to use the standardized priority framework, and recent IHS communications have reaffirmed that cancer-related services—screening, diagnostics, and treatment—fall within the highest priority tier when clinically indicated.[54] In principle, this places oncology services at the top of the allocation framework rather than in lower, discretionary categories.
For tribes operating under self-determination or self-governance authorities, PRC-related policies can look different. While IHS’s medical-priority structure is available as a template, tribally operated health systems are not required to adopt it verbatim. Instead, they may design their own priority frameworks or modify the IHS levels to reflect local values and needs.[55] For example, by explicitly defining how early diagnostic steps, chronic conditions, or behavioral health services are sequenced alongside acute care. In practice, some self-governance tribes mirror IHS priorities for ease of coordination, while others use broader or more flexible categories that emphasize prevention, timely diagnostics, or specific high-burden conditions. This flexibility means that, for PRC pathways, patients may experience different decision rules in IHS-operated facilities compared with tribally operated health programs.
In addition, local interpretation of medical priority criteria shapes how quickly requests move across both IHS-operated and tribally operated systems. Tribes have used consultation, comment letters, and congressional testimony to request clearer guidance and training on how medical priority criteria are applied—particularly where delays can affect time-sensitive care pathways.[56]
Experiences in other clinical areas also illustrate how prioritization can affect timing when conditions are serious but not immediately life-threatening. One Rosebud Sioux patient, for example, reported being denied or waitlisted for PRC funding more than a dozen times since 2018 for an orthopedic problem her physician believed required specialist care.[57] She described living for roughly two years with pain severe enough to require help with daily tasks and believed earlier intervention would have prevented worsening and reduced overall costs.[58] While not a cancer case, it illustrates how the application of medical priority rules may delay treatment for progressive conditions.
PRC referral management describes how a patient’s need for outside care moves from initial IHS or tribal patient registration to final PRC claims payment. After a patient is registered, referrals for non-IHS or non-tribal services are initiated and routed by IHS or tribal providers, then reviewed by PRC staff to determine eligibility, medical priority, alternate-resource use, and authorization decisions as described in the prior section. This section outlines the key steps in that process—patient registration, referral initiation and routing, PRC referral review and authorization, PRC payment and claims processing, and referral denials followed by reconsideration or appeals. Last, this section describes how these functions interact to determine whether and how PRC pays for a given episode of referred care. Figure 2 provides an overview of the PRC process.
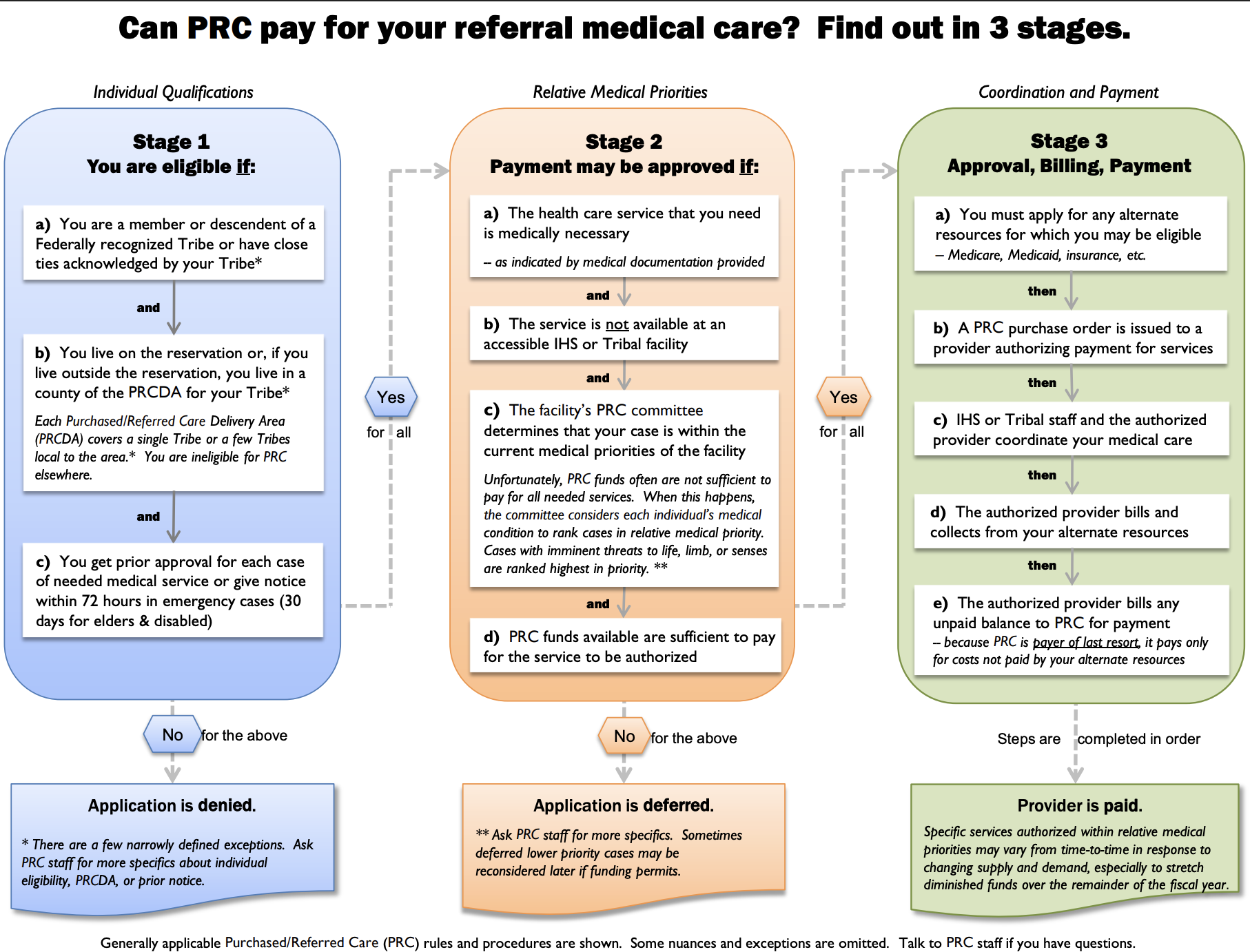
Figure 2. Purchase and Refer Care Eligibility Chart by IHS.GOV.[59]
At each clinic visit, the Service Unit or tribal health program’s patient registration office confirms or updates the individual’s record. The individual is responsible for supplying the following:
1. current mailing and residential addresses;
2. telephone numbers for scheduling and follow-up;
3. emergency contacts; and
4. documentation of tribal citizenship or descent needed for IHS or tribal direct care eligibility.
This registration process is also intended to capture or update information on alternate resources, as previously discussed.[60]
When a face-to-face direct care visit results in the need for services outside the IHS or tribal facility, the clinician issues a referral that is routed to the IHS Service Unit PRC team or the tribal program’s PRC office, respectively. The IHS Service Unit PRC team typically consists of PRC clerks, benefits coordinators, and case managers who work with clinicians to review referrals and determine whether PRC authorization can be issued. In tribally operated programs, PRC teams may include similar roles (e.g., referral/PRC clerks, benefits coordination staff, and case managers), depending on program size and staffing.
A referral is treated as complete when it includes the core information PRC staff need to evaluate eligibility, medical necessity, and coordination of benefits. In most programs, a complete referral: 1) identifies the patient and any known alternate-resource coverage; 2) specifies the requested service and includes clinical information supporting medical need; 3) states the number of visits, days, or units and a brief description of the services requested; 4) names the non-IHS or non-tribal provider or facility; and 5) includes a date of service or date span, when known.[61] Referrals that lack key elements may be considered incomplete and can result in follow-up requests for information or delays in PRC review and authorization. Once a referral is complete, referral routing is initiated.
After a referral is initiated, the PRC administrative team at the Service Unit or tribal health program verifies key requirements, including baseline PRC eligibility, PRCDA residency, notification timelines, completeness of referral documentation, and the status of any alternate resources. Once this initial screening is completed by the PRC administrative team, the case is forwarded to the Service Unit PRC Review Committee (or its tribal equivalent) to determine whether the requested service will be authorized under PRC and eligible for payment, subject to compliance with PRC requirements.[62]
The Service Unit PRC Review Committee is typically composed of clinical and administrative representatives—such as physicians, nurse case managers, PRC staff, and business-office or finance personnel—who are responsible for applying PRC policies to individual cases in light of available funding. Upon receipt of a referral request, the Committee reviews the referral information, confirms the assigned medical-priority level, and determines whether PRC can support payment for the requested services. The Committee may authorize the referral, generally by issuing a written authorization number and defining the scope of approved services (for example, specific procedures, a set number of visits, or a defined date range). It may also deny or defer the request. See section titled, “Referral Denials, Reconsiderations, and Appeals” for more information.
Once a referral is authorized, the PRC program issues a purchase order or payment authorization that specifies the approved provider, services, units (or date span), and any limits or conditions. The outside provider renders care and then submits a claim to IHS for the authorized services, because PRC pays after the primary payer according to coordination-of-benefits rules. This claim typically includes: 1) the PRC purchase‐order or authorization number, 2) itemized charges and clinical coding, and 3) the explanation of benefits (EOB) from any alternate resource billed first.[63]
For IHS-operated PRC programs, authorized outside-provider claims are reviewed and processed for payment by the IHS fiscal intermediary (Blue Cross and Blue Shield of New Mexico). Specific pricing rules apply to PRC. For example, pricing rules may include Medicare-like rates (MLR) for hospital and certain facility services, PRC rates (where applicable), or other established methodologies consistent with regulation and IHS policy.[64] The intermediary verifies that the claim matches the scope of the authorization (correct provider, service, units, and dates), that any required referral or notification documentation is on file, and that primary coverage has been billed.[65] If the claim is complete and consistent with the authorization, the intermediary issues payment to the provider. The intermediary also generates a remittance advice that shows the allowed amount and summarizes how the claim was processed. If any billed items fall outside the authorization or do not meet applicable billing or coverage requirements, the remittance advice will reflect those items as nonpayable charges (i.e., “disallowances”).[66]
Timelines for issuing authorizations and making payments are defined in federal PRC regulations and implementing IHS policy. After IHS receives a qualifying notification from a provider, the program must issue either a purchase order or a denial within five working days.[67] When a complete (“clean”) claim is received for an authorized service, payment is generally expected within 30 days.[68] If documentation is missing (for example, the EOB from an alternate resource) or the billed service exceeds the authorized scope (for example, extra units or an additional procedure not included in the authorization), the claim may be pended for additional information, partially paid for the authorized portion only, or denied with a written notice explaining the reason and the applicable appeal or reconsideration rights under PRC rules.[69]
For tribally administered PRC programs operating ISDEAA, claim payments are managed under the tribe’s approved PRC policies and procedures—such as local pricing agreements, vendor enrollment processes, and internal timelines—so long as those procedures are consistent with federal law and regulation. In both IHS-operated and tribally operated settings, however, the core sequence remains the same: authorization → primary payer (if any) → PRC review and pricing → payment or written notice.
If a denial is issued, the written notice identifies the reason(s), which commonly include notification timing, medical-priority determination, eligibility for IHS direct care, availability or required use of alternate resources, Indian descent or membership status, and residency.[70] If a request is deferred rather than denied, the Review Committee does not issue a final decision but instead places the case on hold—often pending additional documentation, completion of an alternate-resource application, or the availability of PRC funds—with the understanding that the referral may be reconsidered when the specified conditions are met.
If PRC payment is denied, the individual is notified in writing and may request reconsideration within 30 days of receiving the denial letter by writing to the Service Unit Chief Executive Officer.[71] If the outcome remains unchanged after reconsideration at the Service Unit level, the individual may appeal to the IHS Area Director and then to the IHS Director. The IHS Director’s decision constitutes final administrative action. Appeals procedures and timelines may differ for tribally administered PRC programs operating under ISDEAA. In such cases, individuals follow the appeals process specified by the tribal health program.
PRC operates within a broader framework of federal oversight and tribal advocacy. Federal agencies review PRC administration through audits, evaluations, and policy guidance that assess how well program rules are implemented and whether funds are used as intended. At the same time, tribes and tribal organizations use consultation, testimony, and formal correspondence to request improvements in PRC oversight and administration, including clearer guidance, more consistent application of rules, and stronger protections for patients. The subsections below summarize key federal oversight findings and describe how tribal leaders and organizations have called for changes in PRC oversight to better align the program with tribal priorities and patient needs.
Federal reviews have identified recurring challenges in the administration of PRC. In April 2020, the HHS Office of Inspector General (OIG) audited 802,470 PRC claims paid between October 2013 and June 2016, totaling $672.4 million, and drew a random sample of 100 claims to test compliance with nine federal requirements.[72] Tribally administered PRC programs were not part of the review as the audit covered only IHS-administered PRC services.
OIG reported that 18 of the 100 sampled claims complied with all applicable federal requirements, while 82 did not meet one or more standards, such as beneficiary-eligibility documentation, medical-necessity and priority review, timely notification, adherence to PRC’s payer-of-last-resort rule, and timely approval or payment.[73] Based on this sample, OIG estimated that more than 80 percent of the 802,470 paid claims were not reviewed, approved, or paid in full in accordance with applicable requirements of the IHS-administered PRC program.[74]
The audit also examined IHS’s Referred Care Information System (RCIS)—an electronic system used to route referrals and maintain PRC records—and identified control gaps. OIG found that RCIS permitted records to advance without required eligibility documentation and OIG recommended system edits to enforce residency proof at intake.[75] In response to these findings, IHS stated that it concurred with OIG’s recommendations and reported the following actions to address OIG’s review:
1) incorporating residency-verification steps into PRC workflows;
2) providing staff training on medical priority and alternate resources;
3) conducting outreach regarding emergency-notification timelines; and
4) clarifying Indian Health Manual and operational guidance on documentation and payment timeliness.[76]
Earlier federal oversight reached related conclusions about data quality and management. In 2011, the Government Accountability Office (GAO) reported that data used to estimate Contract Health Services (CHS—the precursor to PRC) “need” were incomplete and inconsistent, noting practices that could distort denial counts and hinder reliable estimates.[77] GAO found, for example, that IHS doubled certain categories of reported denials to compensate for missing data and recommended improvements in data quality, program management, and provider communication.[78]
In response, IHS initiated several actions, including establishing an Unmet Needs Data Subcommittee to examine how unmet need is defined and measured for CHS/PRC. The subcommittee’s purview included reviewing data sources and methods, assessing how denials and deferrals are recorded, and advising on options to improve estimates of unmet need. IHS also explored replacing simple tallies of denials and deferrals with a Federal Disparity Index (FDI) approach, which uses an index to compare the level of resources available to IHS and tribal health systems with a benchmark level of funding, thereby estimating the gap between current resources and estimated need. FDI (also described as “Level of Need Funded”) has since been used by IHS in the Indian Health Care Improvement Fund (IHCIF) methodology.[79] Finally, IHS updated its PRC manual guidance to standardize how deferred and denied services are recorded and how unmet need is estimated, drawing on data from the fiscal intermediary (the contractor that processes PRC claims and maintains detailed claims records) and standardized reporting from IHS Areas and tribal health programs.[80] Using both claims-level data and standardized area/tribal reports is intended to improve consistency and comparability across sites and to strengthen the basis for planning and resource allocation.[81]
In addition to federal oversight review, tribal governments request stronger accountability and transparency in PRC administration. In May 2024, the Honorable Cindy Marchand, Secretary, Confederated Tribes of the Colville Reservation in north-central Washington State, testified before the House Appropriations Subcommittee on Interior, Environment, and Related Agencies, requesting that GAO investigate IHS’s administration of PRC at IHS-managed (direct-service) facilities.[82] The Colville Tribes—served by IHS as a direct-service tribe—reported that persistent mismanagement of PRC funds and processes had led to significant lapses in care, including patient deaths. The Tribes described a case in which a Colville tribal elder needed a referral for ongoing cardiac issues but was unable to obtain timely follow-up because calls were not returned and the PRC purchase order was not issued. Despite repeated attempts and escalation to tribal leadership, the referral remained pending, and the elder died of a heart attack before obtaining access to referred care.[83]
From approximately 2017 to 2022, the Portland Area IHS Office administered the PRC program for the Colville Service Unit remotely, using Area Office staff located in Portland, Oregon, rather than on-reservation personnel—approximately 335 miles away.[84] The Colville Tribes further reported that the Portland Area IHS Office imposed documentation requirements beyond IHS regulations or handbook guidance, for example, the office’s annual submission of utility bills, blood quantum, and enrollment proof for tribal elders seeking referrals. Individuals unable to meet these additional requirements either went without care or obtained care on their own and then faced debt collection when IHS declined payment.[85]
Marchand’s testimony also stated that, during the five-year period of Portland-based administration, thousands of PRC purchase orders accumulated without reconciliation (i.e., being reviewed, matched to claims, and formally closed in PRC records). From 2017-2022, the Tribes estimated that approximately $24 million of the Portland Area’s $33 million (about 73%) in PRC “carryover” reflected unresolved Colville cases—either as unobligated balances or as open obligations (e.g., purchase orders that have not yet been fully processed, paid, or closed).[86] The Colville Service Unit attributed this carryover balance primarily to unreconciled PRC purchase orders rather than to surplus funds.[87] In other words, the “carryover” figure did not necessarily indicate that PRC had money left over; it largely reflected a backlog of purchase orders that were still open or not fully processed, which can obscure whether funds are truly available for new referrals.
Marchand additionally testified that private providers began withdrawing from PRC participation, meaning they stopped accepting PRC authorizations or billing IHS/PRC. Their withdrawal reduced local network options for patients and, according to Marchand, contributed to delays and longer travel distances for care.[88] For these reasons, the Tribes urged Congress to direct GAO to conduct another formal review of IHS PRC management at IHS-managed service units, and to ensure that affected tribal governments are directly consulted in the process. As of the date of this report, GAO has not initiated a review.
Recent legislative proposals and federal initiatives have focused on changes to PRC administration, billing practices affecting PRC-approved patients, and mechanisms for incorporating tribal input into PRC policy. This section highlights three examples: 1) H.R. 1418, the Purchased/Referred Care Improvement Act of 2025, which would modify PRC statutory authority and reporting requirements; 2) the Indian Health Service Director’s Workgroup on Improving Purchased/Referred Care, which convenes tribal and federal representatives to review PRC operations and develop recommendations; and 3) a 2024 joint communication from IHS and the Consumer Financial Protection Bureau (CFPB), an independent bureau within the Federal Reserve System, addresses billing and collections practices involving PRC-approved patients. Together, these efforts illustrate how Congress, federal agencies, and tribes are engaging with PRC’s current structure and identifying possible changes through legislative, administrative, and consultative processes.
Recent congressional activity has included proposals to strengthen accountability standards for PRC billing and reimbursement.[89] The Purchased/Referred Care Improvement Act of 2025 (H.R. 1418), introduced in the 119th Congress, would amend section 222 of the Indian Health Care Improvement Act. H.R. 1418 would require HHS to reimburse patients for out-of-pocket costs on PRC-authorized services within 30 days of receiving proper documentation, such as proof of payment.[90] The bill reflects recognition that patients may pay bills themselves to avoid collections while waiting for PRC payments to be processed. The bill requires reimbursement within a defined timeframe, and thus seeks to eliminate prolonged financial risk and ensure that the federal government, rather than patients, bears the cost of approved services. If H.R. 1418 is enacted as-is, patients utilizing PRC would face reduced financial exposure and receive reimbursement for out-of-pocket costs on a more predictable timeline.
The reimbursement provision in H.R. 1418 would not automatically apply to PRC programs operated directly by tribes under ISDEAA compacts or contracts. The bill specifies that these tribal PRC programs are included only if a tribe expressly agrees to adopt the reimbursement procedures.[91] In that sense, the bill primarily governs IHS-administered PRC, while providing an option for tribally operated programs to opt in.
The IHS established the Director’s Workgroup on Improving Purchased/Referred Care in 2010 to strengthen federal–tribal collaboration and provide formal recommendations to the IHS Director on strategies to improve PRC operations, data, oversight, and transparency.[92] The Workgroup reviews input from tribal leaders and other stakeholders to identify program inefficiencies, evaluates the formula used to distribute PRC funds, and recommends operational improvements across IHS and tribal health systems. The Workgroup also functions as an ongoing forum where tribal and federal representatives can discuss PRC eligibility, referral, and payment practices and develop advisory recommendations.
Membership includes two federal or tribal representatives from each of the 12 IHS Areas, providing broad regional representation.[93] The Workgroup typically convenes two times per year.[94] Formal recommendations are submitted to the IHS Director, and once approved, are communicated publicly through “Dear Tribal Leader” letters or similar communications.
On December 12, 2024, the CFPB and IHS issued a joint letter reiterating that individuals whose services are authorized through PRC are not responsible for associated patient cost-sharing (for example, co-pays or deductibles) for those authorized services.[95] The joint communication clarified expectations for providers while reinforcing existing protections for PRC-authorized care. Specifically, the letter notified providers and collectors that attempting to bill or collect from PRC-authorized patients may violate federal law and credit reporting standards, including the Indian Health Care Improvement Act, the Fair Debt Collection Practices Act, and the Fair Credit Reporting Act.[96]
This letter followed a CFPB report released the same day, which found that Native American communities are almost twice as likely as the general population to have medical debt in collections and that these debts are on average 33 percent higher for Native American communities.[97] The report attributed these figures in part to improper billing and delayed PRC payments, which can push authorized debts into collections even when patients are not responsible.
Cancer is an increasingly prominent public health priority in Indian Country. In July 2025, Robyn Sunday Allen (Cherokee Nation), CEO of the Oklahoma City Indian Clinic, stated that “cancer has become the new diabetes in Indian Country.”[98] This section first summarizes the national cancer burden among AI/AN populations, then provides Oklahoma-specific context for tribal communities statewide. It then outlines data collection consideration and how cancer statistics for AI/AN populations are generated, interpreted, and compared across regions and over time. It also describes insurance, economic, and geographic factors that shape cancer outcomes.
Across the United States, non-Hispanic American Indian and Alaska Native (NH AI/AN) populations experience higher cancer incidence, later stage at diagnosis, poorer survival, and
more limited access to medical care than non-Hispanic White (NHW) populations.[99] Analyses report elevated incidence for several sites—including lung, colorectal, liver, stomach, kidney, and cervix—alongside higher proportions of advanced-stage disease and lower survival for many of these cancers.[100]
Regional variation in cancer incidence and mortality further illustrates differences in cancer burden among NH AI/AN communities. CDC data from 2025 indicates that “[t]he overall rate of getting cancer is more than twice as high among NH AI/AN people in the Southern Plains region (612 per 100,000 people) compared to the Southwest region (294 per 100,000 people).”[101] Patterns of cancer type also differ by region. Lung cancer is the most frequently diagnosed cancer among NH AI/AN populations in nearly every IHS region, except the Southwest, where it ranks fourth after colorectal, kidney, and liver cancers. Stomach cancer also shows notable regional variation—ranking fourth among NH AI/AN people in Alaska but only sixth in the Southwest and not appearing among the top ten cancers in several other regions.[102]
According to the 2024 Cancer Burden in the State of Oklahoma, the state’s overall age-adjusted cancer incidence rate is comparable to the U.S. average (~1.2% difference), yet its mortality rate is 19.6% higher. This data suggests a gap between diagnosis and survival outcomes.[103] For example, one Oklahoma-based study noted that the 33 states report higher incidence, and of that number, three report higher mortality—demonstrating the possibility of an incidence–mortality gap.[104]
Oklahoma is home to 38 federally recognized tribes and the country’s largest AI/AN alone population (14.2%).[105] AI/AN alone means that an individual only identifies as American Indian or Alaska Native and not another race. If including AI/AN alone or in any combination, meaning an individual identifies as both AI/AN and another race(s), the state has the second-largest AI/AN population in the United States, after California (9.1%).[106]
Between 2014 and 2018, 9,852 new cancer cases and 2,995 cancer deaths were recorded among the state’s AI/AN population.[107] As an example, by comparison, the age-adjusted cancer incidence rate for NH AI/AN residents was 612.6 per 100,000, compared with 439.9 per 100,000 for NHW residents—about 1.4 times (≈39%) higher.[108] Mortality rates were higher: 262.8 per 100,000 for NH AI/AN versus 176.5 per 100,000 for NHW—about 1.5 times (≈49%) higher.[109] Prior figures demonstrate a similar pattern: from 2000 to 2018, incidence among NH AI/AN Oklahomans increased by roughly 14%, while NHW incidence remained approximately stable (~–1%); NH AI/AN mortality rose by about 4% and NHW mortality declined by about 14%.[110]
Data limitations—such as racial misclassification in cancer registries and vital records—may also understate AI/AN cancer data. Understanding cancer outcomes relies on consistent and accurate data collection. A key consideration in monitoring AI/AN cancer burden is racial misclassification and under-documentation of AI/AN identity in cancer registries and vital records.[111] If AI/AN patients are recorded as another race in medical records or on death certificates, overall incidence and mortality rates for AI/AN populations may be underrepresented.
The inconsistent classification may contribute to a range of underreporting. For example, one 2014 data analysis reported that inconsistent classification of AI/AN race on death records ranged from 1.2% in one IHS Area to 30.4% in another.[112] Further, linkage of cancer registry data with IHS records showed that 77.6% of AI/AN cancer cases in PRCDA counties and 39% of AI/AN cancer cases in non-PRCDA counties were correctly classified as AI/AN.[113] This suggests that AI/AN race misclassification is substantially more common in non-PRCDA counties, and that cancer burden may be undercounted for AI/AN people—particularly outside PRCDA areas.
To address potential data misclassification, national analyses often limit datasets to NH AI/AN residents of PRCDA counties, where linkage with IHS records improves racial classification.[114] This approach seeks to reduce misclassification bias and improve the credibility of regional comparisons. However, it may exclude AI/AN people living outside PRCDA boundaries, AI/AN individuals who are not citizens of a federally recognized tribe (a political classification), or those who do not interface with IHS or tribal health facilities. Analyses conducted in this way may provide more accurate data for the included population but present a national picture that is less than complete.
Improving data quality typically requires collaboration among tribal health programs, IHS, and state cancer registries, including regular record linkages and feedback processes to correct misclassified or incomplete entries.[115] Tools such as the U.S. Cancer Statistics Data Visualization platform—which integrates data from the Centers for Disease Control and Prevention’s National Program of Cancer Registries and the National Cancer Institute’s Surveillance, Epidemiology, and End Results Program—help illuminate trends by region, cancer type, and sex.[116] But experts suggest ongoing refinement is needed to capture the full cancer burden across Indian Country.[117]
More comprehensive, representative data could provide policymakers with a more accurate understanding of cancer disparities, which in turn may contribute to better-aligned screening, prevention, and treatment resources directed to tribal communities that face additional structural barriers to timely cancer care.[118]
Patterns of health coverage, income, and geography help explain some of the observed differences in cancer incidence, stage at diagnosis, and mortality for AI/AN populations.[119] These factors do not determine cancer occurrence on their own, but they may influence exposure to risk factors, participation in screening, and the timing of diagnosis and treatment, which in turn can shape cancer outcomes.
The HHS Office of Minority Health, drawing on 2024 American Community Survey (ACS) estimates, reports that 16.2% of NH AI/AN people are uninsured (compared with 8.2% in the total U.S. population); about 44.8% have private coverage (compared with 67.2%), and roughly 49.1% rely on public programs such as Medicaid or Medicare (compared with 36.8%).[120] These coverage patterns are associated in the broader cancer literature with differences in preventive care use, cancer screening participation, and timeliness of diagnostic evaluation, which may contribute to higher rates of later-stage diagnosis and poorer survival in many AI/AN communities.
Economic differences may also influence cancer risk and outcomes. According to 2024 ACS estimates, the median 12-month household income for NH AI/AN households was $54,485, compared with $81,604 for all U.S. households—about 33% lower.[121] Nineteen percent of AI/AN families live below the poverty line (versus 8.5% nationally), and unemployment among AI/AN people (7.8%) is higher than the national rate (4.5%).[122] Public health literature suggests that lower income and higher poverty can contribute to cancer disparities by increasing exposure to certain risk factors (e.g., commercial tobacco use, occupational hazards, and food insecurity) and by creating barriers to prevention and early detection (e.g., screening access, transportation, time off work). These same constraints can also reduce a patient’s capacity to initiate and sustain recommended cancer care (e.g., completing diagnostic workup, attending treatment visits, and follow-up), which can affect stage at diagnosis and survival.[123]
Geography may further contribute to cancer disparities, particularly for AI/AN individuals in rural or reservation communities that are far from cancer screening and treatment facilities and may have limited or no access to public transportation. Studies of rural and frontier areas have linked longer travel distances and transportation constraints to lower screening participation, delayed diagnostic workup, and differences in treatment patterns, which can translate into regional variation in cancer incidence and mortality.[124]
When viewed together, coverage, economic, and geographic conditions provide important context for interpreting cancer statistics in Indian Country and for understanding why some tribal communities experience higher cancer burden than others. Other clinical, environmental, and social factors may also contribute to observed differences in incidence and survival rates. These variables shape the environment in which PRC and other referral mechanisms operate; later sections of this report examine how PRC-specific rules interact with these broader factors to influence the timing and continuity of cancer care.
A primary way PRC shapes the cancer pathway is through the PRC medical priority framework. As noted previously, under the PRC medical-priority framework, services are grouped into four categories and ranked by priority. Because cancer screening and oncology-related services fall primarily within Categories A and B, this section describes those two categories in detail.
Within Category A: Preventive and Rehabilitative Services, the current medical-priority levels list Screening Mammogram, Screening Sigmoidoscopy/Colonoscopy, and Lung Cancer Screening Low Dose CT (smoker) as Core (Priority 1): Essential services.[125] Within Category B: Medical, Dental, Vision, & Surgical Services, Cancer Diagnosis/Treatment is similarly designated as Core (Priority 1): Essential.[126] This reflects an explicit policy choice to place both cancer screening and the main components of diagnostic workup and treatment in the highest priority tier when PRC funds are allocated.
From the beginning of the cancer pathway, PRC can shape whether and where screening occurs. When an IHS or tribal clinic does not have on-site capacity for mammography, colonoscopy, or low-dose CT lung screening, a clinician issues a referral to an outside facility. That referral enters the PRC process described earlier in this report: the PRC office verifies baseline eligibility (including residence within a PRCDA), confirms that the requested service is a Priority 1 cancer screening, and determines whether alternate coverage such as Medicaid, Medicare, VA benefits, or private insurance is available. For these planned (non-emergent) screenings, prior authorization is generally expected before the outside appointment, and patients are typically responsible for furnishing residency documentation and information about any insurance enrollment or applications. When screening is performed on-site at an IHS or tribal facility, PRC is not involved in payment, but PRC may still be needed for follow-up services if the facility does not provide downstream diagnostics or treatment.
When a screening test—whether performed on-site or at a PRC-authorized outside facility—shows a concerning result, similar steps apply to diagnostic workup and treatment. Referrals for diagnostic imaging, biopsy and pathology, staging studies, surgery, chemotherapy, immunotherapy, radiation therapy, or other oncology services are reviewed under the same medical-priority and payer-of-last-resort rules.
In combination, PRC rules and workflows provide additional context for interpreting the epidemiologic patterns described earlier. Even when cancer screening and treatment are classified as Priority 1 under PRC guidelines, administrative and funding constraints may still affect the timeliness and continuity of care.
Tribal decision-makers may consider various policy options for consideration that are tribally led and sovereignty-driven strategies. This section offers options that consider ISDEAA authorities; coverage and financial protection; regional collaborations and partnerships; service-delivery models; care coordination, navigation, education, and communication; and sovereignty-driven federal engagement.
In the cancer context, self-determination contracts and self-governance compacts can give tribes tools to reduce avoidable delays within referral pathways. For example, tribes may consider the following:
1. standardizing oncology “clean referral” packets that meet PRC documentation needs up front (PRCDA residency proof, alternate-resource verification, and medical-priority justification);
2. codifying expedited internal timelines from abnormal screen to biopsy and first specialty visit; and
3. formalizing vendor relationships with regional cancer centers (such as bundled rates, scheduling assurances, and rapid-response appointment slots).
Tribes may also choose to dedicate navigation staff to manage handoffs across facilities, link travel and lodging supports to referral milestones, and reinvest third-party revenue (including Medicaid, Medicare, and VA agreements) into screening capacity, diagnostics, and treatment partnerships. These efforts can reduce exposure to PRC bottlenecks and hasten time to care.
Depending on tribal priorities, self-determination and self-governance arrangements may be used to redesign eligibility and referral workflows, cancer navigation, and care coordination functions in ways that reflect local definitions of success.[127] Tribes could rely on compacting and contracting to stabilize staffing, shape oncology partnerships, and structure local responses to high cancer burden.
While final federal funding decisions rest with Congress and federal agencies, tribes may exercise their sovereignty to shape how self-determination and self-governance authority is used in practice. These options could include:
1. negotiating compacts and funding agreements that support oncology-relevant priorities;
2. forming or joining consortia to increase bargaining power with payers and cancer centers; and
3. using tribal consultation, intertribal coordination, and data on referral delays or cancer outcomes to inform federal decision-making.
Tribes may consider how governance, financing, and service design can be organized under tribal control to address cancer-related needs when models are adapted to local infrastructure, workforce, and payer realities.
Intertribal consortia and external partnerships are approaches Tribal Nations have used to expand specialty capacity, pool resources, and shorten the pathway from abnormal screen to treatment, including for cancer care. In different regions, tribes have developed collaborative structures that centralize certain functions—such as specialty contracting, housing and travel, navigation, and data—while maintaining community control over local care. For the 38 federally recognized tribes located in Oklahoma, these models illustrate several possible ways to organize cancer-related services at a regional scale, in parallel with existing PRC processes.
Intertribal consortiums are most often mutually beneficial collaborations or partnerships that can include Tribal Nations, health centers, academic institutions or other organizations working together to achieve shared goals.
For example, the Alaska Native Tribal Health Consortium (ANTHC) is the largest, most comprehensive tribal health organization in the United States, serving a statewide AI/AN population.[128] It operates within the Alaska Tribal Health System as a tribal-governed consortium that partners with regional tribal health organizations and delivers statewide services, including specialty care at the Alaska Native Medical Center and systemwide public health and infrastructure programs.[129] Text Box 1 provides more information on ANTHC.
Alaska Native Tribal Health Consortium (ANTHC) Services and Functions |
ANTHC operates in the Alaska Tribal Health System providing the following services or functions: · Its central facility serves as a multi-specialty referral hospital that provides acute, specialty, primary, and behavioral health services, including oncology and hematology. · It coordinates functions that support specialty care for rural patients, including lodging near the hospital, organized travel support, telehealth connections back to village clinics, and prevention programs. · Its unified governance structure supports growth in third-party billing revenue, longer-term investments in specialty services, and integration of cultural healing practices alongside quality-improvement efforts. |
Text Box 1. Created by Native Nations Center for Tribal Policy Research. Cite: Alaska Native Tribal Health Consortium, “ANMC Fact Sheet: Alaska Native Medical Center: High-Quality, Culturally Sensitive Health Care,” January 2024, https://anthc.org/wp-content/uploads/2025/05/2024-ANMC-Fact-Sheet.pdf.
For cancer care, local tribal clinics conduct screening and initiate workups, the Alaska Native Medical Center provides staging and treatment, and follow-up often returns to home clinics through teleoncology—reducing repeated long-distance trips and clarifying handoffs between community sites and the specialty hub.[130] Elements of this model—for example, centralized contracting and pricing, shared housing and travel support for referred patients, and a consistent teleoncology infrastructure—could be adapted to multi-tribe settings outside Alaska, with adjustments for geography and payer mix.
In another example, the South Puget Intertribal Planning Agency (SPIPA) illustrates a different emphasis: coalition infrastructure organized around cancer control rather than a shared hospital. Founded in 1976 by the Chehalis, Nisqually, Shoalwater Bay, Skokomish, and Squaxin Island Tribes, SPIPA supports cancer-related prevention and control efforts across member tribes, including education, coordination, and community-based programming. SPIPA’s data-guided coalition approach may provide a framework for a statewide or multi-region cancer control network with common metrics, shared navigation capacity, and a joint registry.
SPIPA provides the services listed in Text Box 2.
The South Puget Intertribal Planning Agency (SPIPA) List of Services |
SPIPA provides the following services: · Provides intertribal planning support and direct services, including health programs. · Provides breast and cervical cancer screening and diagnostic services through a consortium of Tribal clinics, supported in part by federal early-detection funding. · Offers a long-range Cancer Control Plan that expands screening (including colorectal campaigns). · Includes navigation services that follow individuals from outreach through diagnostic resolution. · Works to strengthen tobacco prevention and cessation efforts. · Maintains a regional tribal cancer registry to guide planning. · Provides a registry and navigation functions that may shorten delays between an abnormal test and treatment initiation. |
Text Box 2. Created by Native Nations Center for Tribal Policy Research. Cite: South Puget Intertribal Planning Agency (SPIPA), “South Puget Intertribal Planning Agency (SPIPA) - Home,” SPIPA, accessed October 15, 2025, https://spipa.org/; SPIPA, Native Women’s Wellness Program Provider and Patient Navigators Manual (South Puget Intertribal Planning Agency, 2024), https://bytovac.com/dev/wp-content/uploads/2025/09/2024-NWWP-Manual.pdf; SPIPA Comprehensive Cancer Control Program (CCCP), 2024-2034 SPIPA Tribal Cancer Plan: Wellness for Today and for Future Generations; A Framework of Action to Reduce the Burden of Cancer in the Communities of the Chehalis, Nisqually, Shoalwater Bay, Skokomish, and Squaxin Island Tribes (SPIPA CCCP, 2024), https://bytovac.com/dev/wp-content/uploads/2025/09/cancer-plan-2024.pdf.
The number of tribes located in Oklahoma and the range of their health systems could be drawn on to combine elements of these models into an Oklahoma-specific consortium that includes a focus on cancer. One potential starting point could be convening a team of health directors, PRC leads, and finance officers to conduct a brief landscape scan for the purpose of: 1) identifying late-stage “hotspots” (geographic clusters where late-stage diagnoses are concentrated); 2) current referral patterns; 3) vendor participation and gaps; 4) travel burdens; and 5) PRC denial or deferral reasons most associated with oncology delays.
This information could provide valuable insight for tribes who may wish to consider two shared investments that other regions have found useful. For example, an option could be to form a regional cancer navigation team that standardizes PRC paperwork, alternate-resource coordination, and appointment scheduling across hospital partners. Another option could be to form a joint contracting function that negotiates oncology referral agreements—potentially including Medicare-like or PRC-rate terms—on behalf of participating tribes.
Cost-sharing formulas could be based on population, utilization, or equal-share approaches, supported by data-sharing memoranda of understandings and a dashboard tracking intervals from abnormal screen to treatment. Over time, tribes interested in deeper integration could explore more centralized arrangements for functions that benefit from scale while retaining local governance over primary care and prevention. Examples of function include housing, travel coordination, and teleoncology infrastructure.
External partnerships can add clinical depth, research capacity, and financing, complementing intertribal efforts. Examples of external partnerships may include university and nonprofit partnerships.
In Oklahoma, the University of Oklahoma’s Stephenson Cancer Center established the Native American Center for Cancer Health Excellence (NACCHE) to improve cancer prevention and survival for Native American populations through coordinated work in research, outreach and education, training, clinical access, and policy development, grounded in bidirectionality and respect for tribal sovereignty.[131] Related initiatives provided by OU Health include an American Indian cancer navigation program that has served thousands of AI/AN patients and families, linking tribal health systems to specialty oncology care and addressing logistical barriers such as travel and follow-up coordination.[132] Thus, tribes could consider establishing a relationship with OU.
In another example, in Washington, Fred Hutch Cancer Center’s Indigenous Cancer Health Equity Initiative (ICHE-i) and the CANOE Partnership (Cancer Awareness, Navigation, Outreach and Equitable Indigenous Health Outcomes) provide an example of how academic centers and tribes can structure collaborative cancer work.[133] ICHE-i emphasizes Indigenous-led solutions, relational accountability, and alignment of care systems with tribal priorities and ways of life.[134] Although ICHE-i and CANOE are Washington-based, they illustrate an Indigenous-led partnership model that may be informative for tribal leaders in Oklahoma as they consider whether similar collaborations with regional academic cancer centers could support outreach, navigation, and coordinated access to specialty oncology care.
National nonprofit collaborations can also extend capacity for cancer prevention, screening, treatment navigation, and related PRC coordination. One example is the American Cancer Society which has worked with tribal clinics to provide culturally tailored education, film screening events, and navigation support.[135] Another example is the American Indian Cancer Foundation (AICAF), a Native-governed national nonprofit, which focuses on reducing cancer burdens in Indigenous communities through improved access to prevention, early detection, treatment, and survivor support.[136] Its work includes technical assistance and toolkits for tribal health systems and national campaigns, such as the Blue Beads colorectal cancer awareness initiative.[137] These organizations offer examples of how external partners can supply evidence-informed tools, training, and campaign infrastructure while Tribal Nations determine priorities and implementation strategies.
Taken together, the intertribal and external examples above illustrate an assortment of collaboration options that can be tailored to tribal priorities and capacity and that may help address operational challenges in PRC-supported referrals—such as inconsistent documentation, variable alternate-resource coordination, gaps in contracted specialty networks, and disjointed communication across systems. Although these partnerships do not change PRC eligibility rules or federal policy, they may still improve access in practice by reducing administrative burdens in PRC-supported referrals and, in some cases, by expanding alternatives to reliance on PRC for specific oncology services. Depending on the model, collaboration could range from informal coordination (e.g., shared PRC referral checklists, common forms, or data-sharing agreements) to more formal shared functions (e.g., a multi-tribe registry and navigation network that tracks referral completion, or joint contracting and travel/housing supports that stabilize access to oncology providers). Where tribes choose to coordinate these PRC-adjacent functions across systems, patients may experience more consistent referral pathways and fewer administrative delays, even while PRC authorization remains case-specific.
Physical distance between patients’ communities and oncology or other specialty facilities remains one of the most consistent barriers along the cancer pathway for tribal citizens. Service-delivery approaches exist to address this barrier, including mobile screening units, shared satellite clinics, and teleoncology. Mobile units bring screening services directly to communities for limited, scheduled visits using a staffed vehicle equipped for preventive care. Satellite clinics extend an existing health system’s footprint by offering periodic in-person specialty services at a secondary site closer to patients (often through rotating specialists or shared clinic space). Teleoncology uses telehealth to connect patients and local care teams with oncology specialists for consultation, treatment planning, and follow-up, reducing the need for repeated long-distance travel.
In practice, these models can complement PRC by reducing travel demands and helping referrals progress more efficiently—for example, by enabling local diagnostic workup or follow-up visits that support timely completion of PRC-authorized care. Service-delivery models that bring screening and oncology services closer to tribal communities offer practical ways to reduce distance barriers and support continuity of care across PRC-supported referral pathways.
Mobile screening units bring preventive services (e.g., mammography or low-dose CT lung cancer screening) directly to communities for scheduled events or rotating clinic days. By reducing travel demands and lowering logistical barriers to screening, mobile units may increase uptake of early detection services and support more timely progression from an abnormal result to diagnostic follow-up. When follow-up requires specialty imaging, biopsy, or oncology consultation outside local facilities, mobile programs can also be paired with navigation and benefits coordination to help patients complete referral paperwork, verify alternate resources, and prepare for PRC-related authorization steps. Table 1 provides examples.
Selected Examples of Mobile Cancer Screening Initiatives These examples illustrate how mobile units can expand access to cancer screening for tribal citizens. |
|
OU Health Stephenson Cancer Center in partnerships with Tobacco Settlement Endowment Trust (TSET) and Other Funders |
· Created mobile screening initiatives as part of a broad strategy to expand access to cancer prevention and early detection. · Provided local screening services to reduce transportation barriers to early detection. · Launched a mobile lung cancer screening unit equipped with low-dose CT technology. |
OU Stephenson Cancer Center & Native American Center for Cancer Health Excellence under the Improving Cancer Outcomes in Native American Communities (ICON) Grant |
· Collaborates with Tribal Nations, such as Cherokee Nation, to deliver lung cancer screening. · Seeks to use the mobile unit during targeted outreach events within tribal communities. · Works to integrate mobile units with navigation pathways for resource deployment. |
Nottawaseppi Huron Band of the Potawatomi (NHBP) |
· Partnered with American Indian Cancer Foundation (AICAF), to host Indigenous Pink Day screening providing same-day mammograms in a community setting. · Worked with navigation and coverage programs to support women who require follow-up imaging or treatment. Mobile teams were integrated into tribal clinic operations, enabling PRC or alternate-resource checks at registration and facilitating conversion of abnormal screens to diagnostic workups with limited delay. |
Minnesota, the Fond du Lac Band of Lake Superior Chippewa & Park Nicollet Health System |
· Used a mobile mammography bus at reservation clinics in Duluth and Cloquet. · Supported dozens of completed mammograms in a single deployment through outreach and scheduling efforts. · Integrated mobile teams into tribal clinic operations, enabling PRC or alternate-resource checks at registration and facilitating conversion of abnormal screens to diagnostic workups with limited delay. |
Table 1. Created by Native Nations Center for Tribal Policy Research. Cite: OU Health, “Early Detection on Wheels: OU Health Stephenson Cancer Center and TSET Bring Life-Saving Lung Cancer Screenings to More Oklahomans,” OU Health, February 14, 2025, https://www.ouhealth.com/blog/2025/february/early-detection-on-wheels-ou-health-stephenson-c/; Katie Halloran, “First Mobile Mammography Unit Books Every Appointment at NHBP,” The Nottawaseppi Huron Band of the Potawatomi, October 19, 2023, https://nhbp-nsn.gov/blog/first-mobile-mammography-unit-books-every-appointment-at-nhbp/; CDC: Centers for Disease Control and Prevention, “Fond Du Lac Keeps Mammograms a Priority During Pandemic,” National Comprehensive Cancer Control Program, September 26, 2024, https://www.cdc.gov/comprehensive-cancer-control/success-stories/fond-du-lac-mammograms.html.
Some tribes working collaboratively with their partners have organized regular specialist outreach to tribal facilities, often described as a satellite clinic. In these models, oncology providers travel to a tribal clinic or shared satellite site on a predictable schedule for consultations, treatment planning, survivorship visits, and, in some cases, selected infusions. In this model, surgery, radiation, and complex chemotherapy continue at regional cancer centers.
One Oklahoma example is the Absentee Shawnee Tribal Health System, which lists oncology among its specialty clinic services, including an oncology physician providing care at the Little Axe Health Center—illustrating how some oncology touchpoints can be brought into a tribal clinic setting rather than requiring every visit to occur at a distant cancer center.[138] More broadly, rural oncology literature describes satellite chemotherapy infusion centers as one strategy to reduce distance barriers. For example, Martha’s Vineyard Hospital in Massachusetts partnered with the Massachusetts General Hospital Cancer Center to operate a satellite chemotherapy infusion center for island residents—illustrating how a smaller community hospital can extend oncology treatment access through a formal relationship with a larger regional cancer center.[139]
The outreach model functions most effectively when framed by clear agreements:
· which entity orders labs and imaging,
· how results are transmitted,
· what payment terms apply (for example, Medicare-like or PRC rates where appropriate), and
· how PRC authorizations are written to cover typical diagnostic cascades rather than single steps.
When a single tribe does not have sufficient space or volume for an on-site clinic, intertribal agreements can identify a shared satellite location, with costs apportioned according to population or expected utilization.
Teleoncology adds a third service-delivery option and is often an addition to existing clinic infrastructure. A common pattern for teleoncology delivery is for laboratory tests, imaging, and nursing assessments to occur at the tribal clinic, while the oncologist connects by secure video for consultations, regimen adjustments, and survivorship care. In-person visits are reserved for infusions, radiation, or procedures at the referral center.
In Alaska’s interior, for example, the Tanana Chiefs Conference—a tribal health consortium serving Alaska Native and American Indian people across a 235,000-square-mile service area—has partnered with Intermountain Health to bring oncology care closer to home.[140] Prior to having a telehealth option, many of these patients traveled long distances (over 350 miles) to Anchorage for repeated appointments. Under this model, patients typically receive initial in-person oncology services in Fairbanks; subsequent chemotherapy, infusion therapy, lab work, imaging, and follow-up consultations are provided locally, with an oncologist participating via telehealth.
Across mobile, satellite, and teleoncology models, follow-up and care coordination are central to effectiveness, particularly when a screening identifies a potential cancer. Effective programs may perform the following functions:
· Treat mobile events and satellite days as components of a single, pre-planned pathway: participants are pre-registered; PRCDA residency, tribal citizenship or descent, and alternate-resource status are verified in advance; orders are written with diagnosis codes that align with payer rules.
· When a screening result is abnormal, standing protocols convert the case to diagnostic evaluation without requiring a new referral.
· Where local policy allows, PRC authorizations are written to cover a standard sequence—confirmatory imaging, biopsy and pathology, and staging—within defined time frames and units, instead of approving each service separately.
· When PRC or cancer navigators are present during mobile and satellite sessions, they can help collect documentation, coordinate benefit verification, confirm PRC eligibility, schedule follow-up appointments, and arrange transportation or lodging if subsequent steps occur off-site.
Coordination practices may help address gaps and reduce the disconnect between screening and treatment by ensuring that patients diagnosed through mobile or outreach services have a clear pathway into diagnostic follow-up and, when needed, treatment. Rather than operating in parallel, PRC processes can be integrated into the same screening-to-diagnosis workflow—for example, by embedding eligibility checks, alternate-resource verification, and authorization preparation into pre-registration and follow-up scheduling.
Further, depending on tribal priorities and local infrastructure, layering service-delivery options could be considered. One configuration might include: 1) clinic-anchored screening and navigation as the foundation; 2) periodic mobile deployments to reach outlying citizens; a visiting-oncologist clinic for consultations and selected therapies; and 3) teleoncology to manage intervals between in-person visits. For tribes that do not own mobile units or specialty clinics, when appropriate, similar models can be pursued through partnerships with neighboring tribes, health systems, or nonprofit organizations that already operate mobile imaging or outreach programs, with PRC coordination and shared protocols built into agreements.
The implementation and expansion of mobile, satellite, and teleoncology models may allow for the following: 1) an increase in the number of tribal citizens who can be screened closer to home; 2) the completion of diagnostic workups in a more effective and timely manner; and 3) the initiation of treatment with standardized workflow, documentation, and payment terms for fewer PRC-related delays. If current arrangements remain unchanged, many patients will continue to navigate distance, fragmented scheduling, and case-by-case PRC approvals, with ongoing risk of delayed diagnosis or treatment.
PRC eligibility, notification timelines, alternate-resource coordination, and medical-priority rules create a multi-step process that may be difficult for tribes and individuals to follow without clear guidance.[141] Although IHS publishes flowcharts to assist patients and staff, variation in local materials and workflows is known to contribute to missed authorizations, preventable denials, delays in care, and, in some cases, avoidable medical debt.[142]
To help address this, tribal programs may use a range of approaches to provide clear guidance to individuals about the PRC process. Some provide concise overviews, such as the Fort Yates IHS Clinic’s brief handout,[143] while others furnish more comprehensive guidance, including the Absentee Shawnee Tribe of Oklahoma’s 20-page PRC guidelines.[144] The Peter Christensen Health Center offers a step-by-step booklet and directs patients to named PRC staff for assistance.[145] The Little Traverse Bay Bands of Odawa Indians maintain a dedicated PRC department with multiple staff who assist with eligibility documentation, referrals, and coordination of benefits.[146] Across these examples, common elements include standardized information, clearly identified points of contact, and assistance with required documentation.
In oncology pathways, timeliness and sequencing may be considered especially important. Opportunities to address timeliness and sequencing could be through education and navigation functions, which may be most effective when embedded at routine touchpoints—registration, ordering of screening tests, and follow-up on abnormal results. Providing clear educational materials and updated PRC information before issues arise may help streamline processes and optimize efficiency.
Tribes may also consider supplementing IHS materials with plain-language toolkits explaining key terms (such as PRCDA, alternate resources, and medical priorities), short videos demonstrating how to assemble proof documents, and mobile or web forms that pre-screen submissions for completeness before PRC review. Additional outreach—such as clinic-based “PRC 101” sessions, culturally relevant workshops, tribal radio segments, or text reminders—can support adherence to notification and documentation timelines.
Further, dedicated PRC navigation staff can perform several core tasks:
· confirm PRCDA residency and tribal citizenship or descent documentation;
· verify alternate-resource status;
· assemble prior-authorization packets;
· track required notifications for emergency encounters; and
· coordinate explanations of benefits from primary payers before PRC adjudication.
Where standing protocols allow screening orders to transition automatically to diagnostic workups after an abnormal result, navigators (staff who help patients and clinics manage referrals, documentation, scheduling, and payer/PRC steps) can help apply those protocols consistently, reducing duplicative referrals and re-review time. For cancer patients, navigation roles often extend to coordinating appointments across multiple sites, clarifying which services fall under PRC versus other payers, and ensuring that authorizations cover the full diagnostic sequence where policy permits.
A combined approach—clear written materials, repeated education at routine touchpoints, and designated PRC navigation support—can help tribal citizens understand key requirements, submit complete referral packets, and provide needed documentation to the PRC office on time. These supports may reduce avoidable “front-end” administrative problems (such as missing eligibility documentation, incomplete alternate-resource information, or unclear notification/authorization steps) that can trigger rework, deferrals, denials, or delayed scheduling—particularly in complex cancer pathways that involve multiple services and vendors. Federal oversight has documented PRC payment and processing problems tied to incomplete or improperly verified information; strengthening navigation and communication upstream may help reduce similar issues by improving the completeness and accuracy of submissions before they enter PRC review and claims processing.[147]
Tribes may consider, however, that implementing these approaches—individually or in combination—often requires dedicated staffing, coordination across clinics and PRC offices, and sustained funding or reallocation of existing resources. In some settings, tribes may also need to align these investments with broader organizational priorities (e.g., workforce capacity, leadership goals, and long-term planning) or pursue external supports—such as grants, partnerships, or policy changes—to sustain navigation and education functions over time.
Some Tribal Nations have turned to coverage and financial-protection strategies to reduce dependence on PRC and protect citizens from gaps tied to IHS funding constraints. In practice, these approaches have included sponsoring Medicaid or Medicare coverage for eligible citizens of their tribe, assisting with marketplace premiums, or—where feasible—purchasing private group coverage to stabilize citizen access to specialty services.[148] In most cases, these strategies are structured primarily for a tribe’s own citizens, but they can also indirectly benefit other AI/AN patients by preserving limited PRC funds for those without alternate coverage. When implemented, coverage strategies create third-party pathways to care when PRC is exhausted or unavailable, while generating sustainable revenue streams for tribal health systems.[149]
In addition, tribal sponsorship models allow tribes to directly cover premiums, deductibles, or co-payments for their citizens, thereby increasing access to coverage and strengthening tribal health system finances.[150] One common model is Medicaid sponsorship, in which a tribe pays premiums or supports enrollment so that eligible members are covered. Once enrolled, services provided at IHS or tribal facilities are generally reimbursed at 100 percent of the Federal Medical Assistance Percentage (FMAP), meaning the federal government pays the full Medicaid share for those services.[151] This may allow the tribe to reinvest Medicaid revenues locally and preserve PRC dollars for patients who remain uninsured or underinsured.[152]
Another approach is Medicare Part B buy-ins by the tribe. Medicare is a federal program that provides health coverage to people age 65 and older and to certain individuals with disabilities.[153] Part B is voluntary and covers a broad range of medical services and supplies.[154] Under Medicare Part B, a tribe can choose to pay Part B premiums for elders or people with disabilities to help maintain continuous access to oncology-related services that might otherwise rely on PRC authorization.
Beyond Medicare sponsorship, some tribes also use other coverage strategies to strengthen access and financial protection. In states with health insurance marketplaces, premium-assistance programs help uninsured citizens enroll in qualified health plans, creating more predictable coverage for high-cost episodes such as chemotherapy, radiation therapy, and complex imaging. Some Tribal Nations additionally purchase private group coverage for vulnerable individuals to secure a stable physician network and pharmacy benefits that operate independently of PRC.[155]
Tribes considering coverage and financial protections for their citizens may determine:
· who is sponsored, for what types of coverage, and for how long—for example, citizens on a cancer pathway from abnormal screen through treatment completion, elders, or uninsured adults meeting specified income criteria.
· arrangements with state agencies for expedited applications and renewals, internal processes to monitor eligibility changes, and clear rules for when the tribe will cover deductibles or premiums.
· determining how PRC funds, third-party revenues, and tribal appropriations will be braided to sustain sponsorship and administrative capacity over time.
In the cancer context, continuous third-party coverage can shift some routine oncology costs away from PRC and create a more predictable pathway to specialty care when PRC funds are exhausted or unavailable. Continuous third-party coverage can also help shorten the processing time between an abnormal screening result to diagnostic workup (i.e., biopsy, pathology, staging) and initiation of treatment. Because PRC is the payer of last resort, having verified alternate coverage in place can reduce the documentation and coordination steps that would otherwise precede PRC authorization for referred oncology services. Coverage can also facilitate referrals to cancer centers, support pharmacy access for oral chemotherapy and supportive medications, and help maintain follow-up schedules without interruptions tied to PRC funding availability.
While decisions about Medicaid expansion, marketplace design, and federal coverage rules rest with states and federal agencies, tribes may exercise their sovereignty to shape how these coverage tools are deployed for their citizens. Options could include the following:
1) developing or scaling tribal sponsorship programs tailored to cancer pathways;
2) negotiating data-sharing and streamlined enrollment processes with state Medicaid agencies and marketplace entities; and
3) coordinating across tribes to share program designs, administrative tools, and lessons learned.
Collectively, these coverage and financial-protection approaches show how tribally led strategies could be organized to reduce reliance on PRC for routine oncology services, improve timely access to specialty cancer care, and strengthen tribal health infrastructure through sustainable third-party revenue. Implementation of these approaches, however, may depend on sustained funding for premiums and cost-sharing support, administrative capacity to manage eligibility and renewals, and coordination with state and federal partners to streamline enrollment and reimbursement workflows.
Tribal governments routinely engage federal partners to shape how PRC functions in practice. This engagement may occur through the use of IHS budget formulation, tribal consultation (including responding to federal Dear Tribal Leader Letters), comments on proposed rules and manual updates, technical assistance to congressional offices, and testimony before appropriations and authorizing committees. The following topics summarize federal levers that affect PRC’s role in cancer care and describe the program features that tribes may wish to address in those venues.
Through the National Tribal Budget Formulation Workgroup—a 25-member workgroup (typically two tribal representatives from each of the 12 IHS Areas) that develops annual tribal budget priorities and recommendations for IHS funding—tribal leaders annually identify target funding levels they believe are necessary to fulfill the federal trust responsibility.[156] For FY 2026, the Workgroup requested $63.04 billion for IHS overall, with substantial increases to PRC to meet rising specialty-care costs.[157] By comparison, the President’s FY 2026 Budget proposed $8.1 billion for IHS (about $7.9 billion in discretionary funding and $159 million in proposed mandatory funding for the Special Diabetes Program for Indians),[158] and the House Appropriations Committee advanced $8.41 billion for IHS, with $1.054 billion specifically for PRC.[159]
Notably, in 2017, the Government Accountability Office reported that IHS per capita spending for users was $4,078, compared with $8,109 for Medicaid, $10,692 for the Veterans Health Administration, and $13,185 for Medicare.[160] According to analysis by the National Congress of American Indians, IHS funding would need to nearly double to reach parity with the level of care provided to federal inmates, and even greater increases would be required to match benefits offered through Medicaid.[161] These figures describe spending per enrollee or user in each system and are frequently used by tribes to contextualize requests for increased IHS appropriations or to brief congressional staff.
Funding levels interact with timing on the ground. When local PRC funds are strained late in a fiscal year, programs may defer approvals for non-urgent services or carry authorized purchase orders into the next fiscal year for payment. Oncology episodes can be affected because chemotherapy, radiation, advanced imaging, and specialty visits typically occur over many months and require uninterrupted scheduling. Comprehensive national statistics on PRC denials or deferrals attributable specifically to funding availability are not published in a standardized, system-wide format. However, audits and oversight reports have documented instances in which PRC claims were not paid or were processed late, and service units and tribal programs routinely report the need to triage authorizations when resources tighten. In federal engagement, tribes often pair local information—such as the number of oncology purchase orders awaiting funding or cases where referrals could not be approved within the fiscal year—with these national funding and per-capita comparisons.
Depending on tribal priorities, sovereignty-driven federal engagement on IHS and PRC funding can take several forms. One avenue is participation in national and regional budget formulation processes, including nominating representatives to the National Tribal Budget Formulation Workgroup or attending area-level budget meetings, so cancer-related needs—such as PRC for oncology referrals, travel and lodging for treatment, and oncology workforce capacity—are explicitly reflected in recommended funding levels.
A second avenue involves using local PRC and cancer data in outreach to Congress: tribes may compile information on pending or deferred oncology referrals, PRC purchase orders awaiting funding, or time from abnormal screen to treatment and share these data with congressional delegations alongside per-capita comparisons from GAO and other federal sources, as commonly seen in tribal testimony before appropriations subcommittees.
At the federal level, Congressional appropriations for IHS determine the resources available for programs such as PRC.[162] Unlike entitlement programs such as Medicare and Medicaid, IHS—including PRC—has historically been funded through annual discretionary appropriations. When resources tighten within a fiscal year, programs tend to prioritize urgent or emergent cases and pace approvals for non-urgent referrals.[163] Beginning with FY2024 and continuing in FY2026, Congress provided IHS advance appropriations—funding enacted a year ahead so core services can continue during a lapse or shutdown.[164] PRC is included in advance appropriations.[165] While advance appropriations improve operational stability, they do not alter PRC’s discretionary status or close the gap between identified need and available resources. Decision-makers may find this particularly acute in services for oncology, where services are high-cost and time-sensitive.
A longer-term structural question is whether IHS appropriations should remain discretionary or shift, in whole or in part, toward mandatory funding. Under a mandatory model, similar to Medicare or the federal share of Medicaid, funding would be provided on a more predictable basis, which could support multi-year planning, longer-term contracts, and more consistent PRC operations.[166] Retaining purely discretionary status, by contrast, keeps IHS subject to annual negotiations, continuing resolutions, and potential shutdowns, which can introduce uncertainty into PRC referral and payment cycles, and thus uncertainty with continuing services over multiple years, which is often the case with cancer care. Tribes and tribal organizations have engaged on these questions through budget formulation recommendations, written testimony, and consultation comments.
Here, tribes may consider coordination with tribal and national organizations that focus on IHS appropriations and policy, such as the National Indian Health Board, the National Council of Urban Indian Health, and regional health boards. These organizations compile joint testimony, organize sign-on letters, and track appropriations developments; recent advances in IHS advance appropriations reflect this combined tribal and organizational advocacy. Tribes may engage directly in policy discussions about mandatory funding and related reforms by adopting tribal resolutions, submitting comments during formal consultation, or joining national campaigns that support mandatory IHS funding proposals, expanded advance appropriations, or technical changes to PRC accounts. In some cases, tribal leaders have linked these positions to recent court decisions that increase federal obligations for contract support and overhead costs in tribal health programs, emphasizing the importance of stable appropriations to meet those obligations.
From a cancer-care perspective, the implications are straightforward. If sustained tribal engagement contributes over time to higher and more predictable IHS and PRC appropriations, local programs would have greater capacity to authorize and maintain oncology referrals across an entire course of treatment, rather than adjusting approvals in response to mid-year funding constraints. If appropriations remain substantially below identified need, PRC programs are likely to continue relying on strict medical-priority rules and intra-year pacing of authorizations, with potential effects on the timing and continuity of specialty cancer care. Sovereignty-driven federal engagement—through budget formulation, testimony, coalition advocacy, and consultation—does not guarantee specific funding outcomes, but could provide structured avenues for tribes to shape how federal decision-makers understand PRC needs and their relationship to cancer outcomes in tribal communities.
Staffing levels in IHS facilities and PRC offices influence how quickly appointments are scheduled and how referrals are issued, reviewed, and authorized. GAO reported in 2018 that nearly 25 percent of provider positions (physicians, nurses, nurse practitioners, pharmacists, and others) were vacant across IHS, with some service units exceeding 50 percent vacancy.[167] In 2017, turnover rates were 46 percent for physicians and 30 percent for nurses.[168]
PRC processes and patient care may be impacted when administrative capacity is not optimal, which can lead to a patient’s confusion in the referral, approval, and declination process, as well as being left with debt if their PRC is ultimately not approved.[169] Contributing factors include rural locations, limited housing, and challenges matching local market salaries, which can increase reliance on temporary contracted providers and affect continuity of care.
Whether driven by staffing shortages, communication gaps, or other local constraints, these concerns underscore why some tribes emphasize investments in PRC staffing, navigation, and clear points of contact as part of their broader strategies to improve the timeliness and predictability of referred care. Federal workforce tools exist but can be limited in capacity. The IHS Loan Repayment Program (LRP) and IHS Scholarship Program recruit clinicians to underserved sites by tying service obligations to financial support.[170] Demand for awards typically exceeds available slots: roughly 130 new LRP awards are made each year despite nearly double that number of qualified applications.[171] Tribes frequently urge expansion of these programs, data-driven pay flexibilities, and retention incentives through consultation and budget requests. Reflecting the urgency of these concerns, IHS announced on January 29, 2026 what it described as the largest hiring initiative in the agency’s history, signaling a major federal effort to expand hiring capacity, reduce longstanding vacancy pressures, and strengthen retention across priority clinical, public health, administrative, and leadership roles throughout the agency.[172]
Sovereignty-driven engagement on workforce issues can occur on parallel tracks: influencing federal workforce programs and building tribal-controlled pathways. At the federal level, tribes may use consultation, budget formulation, and testimony to highlight vacancies in positions that shape cancer timelines—for example, radiology technologists, oncology nurses, surgeons, and PRC caseworkers. They may also request targeted expansions of LRP and scholarship slots for these disciplines. Tribes can also provide site-specific data on vacancy duration, turnover, and use of temporary contract providers, paired with information on oncology delays, to inform decisions about where new federal workforce investments are most needed.
At the tribal and intertribal level, some governments are developing their own strategies to recruit and retain staff in collaboration with or alongside IHS. Approaches include:
1. establishing tribal or consortium-based workforce pipelines with local colleges and universities (for example, creating health-career tracks for tribal students and clinical rotations at tribal or IHS facilities),
2. offering tribal-funded scholarships or stipends with service expectations in community clinics, and
3. working with nearby health systems to create shared positions or joint appointments that distribute specialty providers across multiple sites.
Housing initiatives—such as tribal housing preferences for clinicians, short-term staff lodging, or partnerships with local housing authorities—have also been used to make rural placements more feasible. For PRC specifically, tribes may choose to fund PRC navigators or case managers as tribal employees, even when the PRC program is federally operated, to ensure that referral packets are complete, eligibility documentation is assembled, and communication with patients is continuous.
If federal and tribal workforce strategies expand in ways that address both recruitment and retention in cancer-relevant roles, IHS and tribally operated facilities may be better able to fill persistent vacancies, reduce reliance on costly temporary providers, and improve timeliness along the cancer pathway. Tribes considering these workforce strategies may need to plan for sustained multi-year funding and administrative capacity, make clear decisions about which roles they can directly support versus those dependent on federal programs, and establish benchmarks to evaluate progress (e.g., vacancy duration, turnover, and downstream impacts on cancer-related referral and PRC timelines). If workforce efforts remain limited, vacancy and turnover rates near historical levels are likely to persist, with ongoing implications for access to primary care, specialty referrals, and PRC processing in tribal communities.
As described earlier in this report, federal policy links PRC eligibility for most non-emergent services to both IHS eligibility and residence within a tribe’s PRCDA.
Individual experiences illustrate how geography interacts with policy. One documented example involved a member of the Little Shell Tribe of Chippewa Indians who lived several hundred miles from her tribe’s headquarters and was ineligible for PRC coverage because her residence fell outside a designated PRCDA, despite her tribal citizenship.[173] She explained that quitting her job and relocating her family back to her reservation would be the only way to gain eligibility.
PRC and Geographic Considerations—Report Highlight: A tribal citizen may live closer to specialty care after relocating for work, education, or family reasons, yet fall outside their tribe’s PRCDA, making PRC authorization unavailable for planned diagnostics and treatment. Conversely, remaining within a PRCDA may preserve eligibility but require repeated long-distance travel for radiation, chemotherapy, or follow-up visits. |
For oncology, where diagnostics and treatment are often located in urban cancer centers, residency requirements can shape whether PRC payment is available for scheduled non-emergent care even when a patient is otherwise IHS-eligible. A tribal citizen may live closer to specialty care after relocating for work, education, or family reasons, yet fall outside their tribe’s PRCDA, making PRC authorization unavailable for planned diagnostics and treatment. Conversely, remaining within a PRCDA may preserve eligibility but require repeated long-distance travel for radiation, chemotherapy, or follow-up visits.
Recent actions demonstrate that PRCDA boundaries can be adjusted through federal redesignation. For example, in November 2024, the IHS published a notice in the Federal Register expanding the Pokagon Band of Potawatomi Indians’ PRCDA to include Kalamazoo, Kent, and Ottawa Counties in Michigan.[174] The expansion increased the Band’s PRC-eligible population by an estimated 537 tribal citizens.[175] In explaining its decision, IHS cited residents’ social and economic affiliation with the tribe, the geographic proximity of the new counties to the existing PRCDA, and the Band’s ability to extend PRC without additional IHS funding.[176] This case illustrates how PRCDA rules are applied in practice and how documentation of affiliation, proximity, and fiscal capacity can support boundary modifications.
Sovereignty-driven engagement around PRCDA parameters could focus on how tribes present information and proposals within this federal framework. Tribes may compile data on:
· where their citizens physically reside;
· patterns of cancer screening, diagnosis, and treatment use in urban and regional centers; and
· the financial and logistical consequences when PRC is unavailable because of residency rules.
They may then use that information in consultation with IHS to request PRCDA modifications—drawing on precedents such as the Pokagon expansion to document social and economic affiliation, proximity to existing PRCDAs, and the tribe’s capacity to operate within current funding levels. In some cases, tribes also brief congressional offices on how PRCDA boundaries affect oncology access for their citizens, particularly when large portions of their population live in metropolitan areas. For states like Oklahoma, where PRCDA already extends statewide, these same tools can be used to support other regions seeking broader PRCDA coverage and to highlight remaining gaps for citizens who move out of state or outside IHS service areas.
As described earlier in this report, PRC authorizations are organized using medical priority levels established in regulation and policy for IHS-operated programs. Sovereignty-driven engagement around medical priorities could operate on two levels. In IHS-operated systems, tribes may focus on how federal guidance is written and implemented—tracking whether priority levels are applied consistently, sharing case examples where serious conditions experienced delays, and recommending clarifications or training to better align PRC practice with clinical timelines.
In self-governance and self-determination settings, tribes can also redesign their own internal PRC policies: developing local priority frameworks, checklists, and pathways that explicitly account for prevention, early diagnostics, and progressive conditions, and then sharing those models with other tribes and with IHS during consultation. From a cancer perspective, the formal elevation of oncology services within the IHS priority structure is a notable policy change. Tribal governments can build on that foundation by shaping how priorities are interpreted, implemented, or reconfigured in their own systems to support timely movement from screening to diagnosis and treatment.
As described earlier in this report, PRC functions as the payer of last resort. Sovereignty-driven engagement on alternate-resource coordination focuses on how to maintain the payer-of-last-resort safeguard while reducing avoidable delays for high-acuity conditions. In consultation and policy discussions, some tribes and tribal organizations have suggested several options:
· One option is provisional PRC authorization for defined episodes of care, with alternate-resource verification and reconciliation occurring in parallel rather than strictly in sequence.
· Another option is clarified authority for PRC to assist with deductibles and coinsurance in specified circumstances once a primary payer has adjudicated the claim.
· A third approach is the use of retrospective review for life-threatening or rapidly progressive conditions where immediate treatment is clinically indicated.
In outlining these ideas, tribes sometimes reference comparable approaches in other federal programs as examples of models that seek to balance timeliness with payer coordination. For example, tribes may reference certain Veterans Health Administration community-care arrangements or emergency Medicaid processes that authorize care while coverage details are finalized.[177] Programs like the IHS Catastrophic Health Emergency Fund (CHEF)—a central fund that provides federal relief for very high-cost cases once a local expenditure threshold is reached—are also referenced as illustrations of how federal policy can accommodate expensive episodes within existing fiscal parameters and reduce pressure on PRC budgets.[178]
If future federal rulemaking or guidance allows for more flexible alternate-resource coordination in narrowly defined situations—such as cancer pathways where delays are clinically consequential—PRC programs could have additional tools to support timely treatment while still ensuring that other available coverage is used first. In the meantime, tribes may choose to focus their engagement on documenting how alternate-resource requirements operate in practice for oncology patients, identifying where coordination works well and where it contributes to delay, and using that information in consultation, comment letters, and local policy design.
This report described how the PRC program is structured and administered, and how its eligibility rules, PRC Delivery Areas, notification requirements, alternate-resource coordination, medical-priority frameworks, workforce capacity, and funding constraints intersect with cancer screening, diagnosis, treatment, and follow-up for tribal citizens. Drawing on national and Oklahoma-specific data, the report highlights that cancer incidence and mortality among AI/AN populations are influenced not only by clinical risk factors, but also by residence patterns, insurance coverage status, and the extent to which referred oncology services can progress efficiently from abnormal screening results to diagnostic workup and treatment initiation. Cancer care experiences vary for many reasons, including local health system capacity, geography, insurance coverage, and care coordination. PRC’s role as the payer of last resort, its reliance on discretionary appropriations, and the complexity of its referral and authorization processes can also affect the timeliness and financial outcomes for some patients, such as delays, denials, or unresolved financial obligations.
This report provides policy options for consideration for tribal decision-makers. Governance and self-determination strategies, including use of ISDEAA authorities, can give Tribal Nations greater control over PRC-related workflows, oncology partnerships, and navigation functions. Coverage and financial-protection approaches—such as Medicaid, Medicare, marketplace sponsorship, and targeted group coverage—offer ways to stabilize access to high-cost cancer services and generate third-party revenue that can be reinvested locally. Regional collaborations and external partnerships can pool referral volume, standardize contracting, and share navigation, housing, and teleoncology infrastructure, while service-delivery models bring elements of cancer care closer to where people live. Strengthened care coordination, navigation, education, and communication can improve how existing PRC rules are applied on the ground, and sovereignty-driven federal engagement provides avenues to influence IHS and PRC funding, workforce tools, PRCDA parameters, medical-priority guidance, and alternate-resource rules over time. In conclusion, these policy options for consideration offer a set of sovereignty-consistent tools that tribal leaders and partners may adapt, combine, or set aside as they determine how best to improve cancer timeliness and outcomes within and alongside the PRC system.
[1] 42 C.F.R. § 136.1 (Definitions), https://www.ecfr.gov/current/title-42/chapter-I/subchapter-M/part-136/subpart-A/section-136.1; 42 C.F.R. § 136.21 (Definitions), https://www.ecfr.gov/current/title-42/chapter-I/subchapter-M/part-136/subpart-C/section-136.21; Indian Health Service, Indian Health Manual, Part 2, Chapter 3, “Purchased/Referred Care,” https://www.ihs.gov/ihm/pc/part-2/chapter-3-purchased-referred-care/. Note: Federal law’s definition of “Indian tribe” expressly includes certain Alaska Native entities, including Alaska Native villages/groups and (for specified purposes) Alaska Native regional or village corporations organized under ANCSA.
[2] Indian Health Service, “Glossary and Terms,” Purchased/Referred Care (PRC), https://www.ihs.gov/prc/glossary-and-terms/.
[3] Snyder Act, 25 U.S.C. § 13, 42 Stat. 208 (1921).
[4] Transfer Act of 1954, Pub. L. Nos. 83–568, 42 U.S.C. (1954).
[5] Indian Health Service, “History,” Purchased/Referred Care (PRC), https://www.ihs.gov/prc/history/.
[6] Indian Health Care Improvement Act (IHCIA), Pub. L. Nos. 94–437 (1976).
[7] Indian Health Service, “Glossary and Terms.”
[8] Indian Health Care Improvement Act (IHCIA) § 201(a)(4), 25 U.S.C. § 1621(a)(4); 42 C.F.R. pt. 136 (2024).
[9] Consolidated Appropriations Act, Pub. L. Nos. 113–76 (2014).
[10] 42 CFR § 136.2 (2024).
[11] 42 CFR § 136 (2024).
[12] Indian Self-Determination and Education Assistance Act, 88 Stat. 2203 (1975); Department of the Interior, Bureau of Indian Affairs and Department of Health and Human Services, Indian Health Service, Public Law 93-638 Indian Self-Determination and Education Assistance Act, as Amended Regulations Final Rule (1996), https://www.bia.gov/sites/default/files/dup/assets/bia/ots/ots/pdf/Public_Law93-638.pdf.
[13] Mariel J. Murray et al., Tribal Self-Determination Authorities: Overview and Issues for Congress, no. R48256 (Congressional Research Service, 2025), https://www.congress.gov/crs-product/R48256; Mariel J. Murray, Indian Self-Determination and Education Assistance Act (ISDEAA) and the Bureau of Indian Affairs, no. IF11877 (Congressional Research Service (CRS), 2024), https://www.congress.gov/crs-product/IF11877.
[14] Indian Health Care Improvement Act Amendments of 1992, Pub. L. Nos. 102–573 (1992).
[15] Tribal Self-Governance Amendments of 2000, Pub. L. Nos. 106–260 (2000).
[16] Indian Health Service, Office of Tribal Self-Governance, “Indian Health Service Tribal Self-Governance Program,” October 2022, https://www.tribalselfgov.org/wp-content/uploads/2022/11/IHS_OTSG_Brochure.pdf.
[17] Indian Health Service, “Tribal Self-Governance Fact Sheet,” July 2016, https://www.ihs.gov/sites/newsroom/themes/responsive2017/display_objects/documents/factsheets/TribalSelfGovernance.pdf.
[18] 42 CFR pt. 137 (Tribal Self-Governance), esp. § 137.7.
[19] ISDEAA Title I self-determination contracting authority, 25 U.S.C. § 5321(a)(1), and implementing regulations at 25 C.F.R. pt. 900; ISDEAA Title V self-governance compacting and funding agreement authorities, 25 U.S.C. §§ 5384–5386 (including funding agreements and redesign/consolidation of programs, services, functions, and activities).
[20] Indian Health Service, “Requirements: Eligibility,” Purchased/Referred Care (PRC), https://www.ihs.gov/prc/eligibility/requirements-eligibility/.
[21] Ibid.
[22] 42 CFR § 136.12 (2024).
[23] Federally Recognized Indian Tribe List Act of 1994, Pub. L. No. 103-454, 108 Stat. 4791 (1994), codified at 25 U.S.C. §§ 5130–5131, https://www.govinfo.gov/content/pkg/COMPS-1398/pdf/COMPS-1398.pdf; 25 C.F.R. pt. 83, Procedures for Federal Acknowledgment of Indian Tribes, https://www.ecfr.gov/current/title-25/chapter-I/subchapter-F/part-83; U.S. Department of the Interior, Bureau of Indian Affairs, “Indian Entities Recognized by and Eligible To Receive Services From the United States Bureau of Indian Affairs,” Federal Register 89, no. 238 (December 11, 2024), https://www.federalregister.gov/d/2024-00109; National Defense Authorization Act for Fiscal Year 2026, Pub. L. No. 119-60 (December 18, 2025)(enacted Dec. 18, 2025; used here as the “as of” date because it included provisions extending federal recognition to the Lumbee Tribe of North Carolina, bringing the total from 574 to 575), https://www.congress.gov/bill/119th-congress/senate-bill/1071/all-info.
[24] 42 CFR § 136.1 (2024). Note: The term “Indian” includes “Indians in the Continental United States, and Indians, Aleuts and Eskimos in Alaska.”
[25] 42 CFR § 136.12 (2024).
[26] 42 CFR § 136.21 (2024).
[27] ArcGIS, “2023 Purchased/Referred Care Delivery Areas (PRCDA),” 2023, https://www.arcgis.com/apps/mapviewer/index.html?layers=328c1fd0043d43ac88ce86b0bf80561f.
[28] 42 CFR § 136.23 (2024).
[29] Indian Health Service, “Glossary and Terms.”
[30] For example, under IHS PRC policy, students and other individuals who are temporarily away from their PRCDA residence may remain PRC-eligible for up to 180 days after departure, subject to all other PRC requirements and documentation, including maintaining their underlying eligibility and providing information needed to confirm their temporary status and current location. See 42 CFR § 136.23 (2024).
[31] U.S. Department of Health and Human Services Office of Minority Health, “American Indian and Alaska Native Health,” Office of Minority Health, September 2025, https://minorityhealth.hhs.gov/american-indian-and-alaska-native-health.
[32] IHS Office of Environmental Health & Engineering, Oklahoma and Texas Purchased/Referred Care (PRC) Delivery Area Map, Indian Health Service, July 2019, https://www.ihs.gov/sites/oklahomacity/themes/responsive2017/images/PRC%20Delivery%20Area%20of%20OK%20July%202019.jpg.
[33] Indian Health Service, “Indian Health Manual - Services to Indians and Other - Chapter 3 Purchased/Referred Care Revisions,” 2018, https://www.ihs.gov/sites/prc/themes/responsive2017/display_objects/documents/IHS_PRC_Chapter_Revisions_2018.pdf.
[34] “Notice of Purchased/Referred Care Delivery Area Re-Designation for the Chippewa Cree Tribe of the Rocky Boy’s Reservation,” Federal Register, June 27, 2025, https://www.federalregister.gov/documents/2025/06/27/2025-11866/notice-of-purchasedreferred-care-delivery-area-re-designation-for-the-chippewa-cree-tribe-of-the.
[35] Ibid.
[36] Indian Health Service, “Glossary and Terms.”
[37] 42 CFR § 136.24 (2024). Note: Federal PRC regulations allow limited flexibility when advance notice is impracticable or when good cause exists, as determined by the ordering official on a case-by-case basis, but sufficient information must still be provided for PRC to assess eligibility and determine whether an authorization/purchase order can be issued.
[38] Ibid.
[39] 42 CFR § 136.203 (2024).
[40] 42 CFR § 136, Subpart C (2024).
[41] 42 CFR § 136.61 (2024).
[42] Indian Health Service, “Requirements: Alternate Resources | Eligibility,” Purchased/Referred Care (PRC), https://www.ihs.gov/prc/eligibility/requirements-alternate-resources/.
[43] Social Security Act, Title XVIII (Medicare), Part A (Hospital Insurance), § 1811, 42 U.S.C. § 1395c; Title XVIII, Part B (Supplementary Medical Insurance), § 1831, 42 U.S.C. § 1395j; and Title XIX (Medicaid), 42 U.S.C. § 1396 et seq.
[44] Indian Health Service, Indian Health Manual, pt. 2, ch. 3, “Purchased/Referred Care,” sec. 2-3.8B (“Eligibility for Alternate Resources”), https://www.ihs.gov/ihm/pc/part-2/chapter-3-purchased-referred-care/#2-3.8B.
[45] Julia Ysaguirre, “2025 Indian Health Service Purchased/Referred Care (PRC) Training,” August 13, 2025, https://www.nihb.org/wp-content/uploads/2025/08/08-Julia-Ysaguirre_Purchased-Referred-Care.pdf.
[46] Indian Health Service, Indian Health Manual.
[47] Ibid.
[48] Note: When funding is sufficient, medical-priority ranking may be less determinative; however, PRC authorizations still require that all eligibility and authorization conditions are met.
[49] 42 CFR §136.23(e) (2024).
[50] Indian Health Service, “Purchased/Referred Care (PRC) | Fact Sheets,” Indian Health Service, December 2024, https://www.ihs.gov/newsroom/factsheets/purchasedreferredcare/; Indian Health Service, “Manual Exhibit 2-3-B: INDIAN HEALTH SERVICE MEDICAL PRIORITY LEVELS,” January 2019, https://www.ihs.gov/sites/ihm/themes/responsive2017/display_objects/documents/pc/58619-1_Manual_Exhibit_2-3-B_IHS_MedicalPrioritiesRolesAndResponsibilities.pdf.
[51] Melanie Anne Egorin, “IHS Testimony on H.R.7516: Improving Purchased/Referred Care,” Department of Health and Human Services, April 30, 2024, https://www.hhs.gov/about/agencies/asl/testimony/2024/04/30/hr-7516-purchased-referred-care-improvement-act-2024.html.
[52] Indian Health Service, INDIAN HEALTH SERVICE MEDICAL PRIORITY LEVELS (2025), https://www.ihs.gov/sites/prc/themes/responsive2017/display_objects/documents/PRC_Medical_Priorities.pdf.
[53] Ibid.
[54] P. Benjamin Smith, “Dear Tribal Leader,” letter, Indian Health Service (IHS), August 20, 2025, https://www.ihs.gov/sites/newsroom/themes/responsive2017/display_objects/documents/2025_Letters/DTLL_08202025.pdf.
[55] Lummi Nation, Purchased & Referred Care (PRC) Policy Manual, October 13, 2020, https://www.lummihealth.gov/wp-content/uploads/PRC-Policy-Manual__OCTOBER-2020.pdf. Note: The Lummi Purchased & Referred Care Manual describes tribe-specific PRC rules, including locally defined PRCDA, program inclusions/exclusions, and locally defined emergency categories.
[56] Janet Alkire, written testimony, U.S. House of Representatives, Committee on Natural Resources, Subcommittee on Indian and Insular Affairs, legislative hearing on H.R. 7516 (Purchased and Referred Care Improvement Act of 2024) and H.R. 2687, April 30, 2024, https://docs.house.gov/meetings/II/II24/20240430/117032/HHRG-118-II24-Wstate-AlkireJ-20240430.pdf.
[57] Rosebud Comprehensive Healthcare Facility Purchased/Referred Care, “PRC Rejection Letter for Constance Celene Brushbreaker,” March 5, 2024, https://www.documentcloud.org/documents/25041017-rejection-letter/.
[58] Arielle Zionts, Katheryn Houghton, “Patients Suffer When Indian Health Service Doesn’t Pay for Outside Care,” KFF Health News, September 5, 2024, https://kffhealthnews.org/news/article/indian-health-service-patients-out-of-network-purchased-referred-care-program/.
[59] Indian Health Service, “Can PRC Pay for Your Referral Medical Care? Find out in 3 Stages,” 2018, https://www.ihs.gov/sites/prc/themes/responsive2017/display_objects/documents/CHSProcessHandout1.pdf.
[60] Julia Ysaguirre, “2025 Indian Health Service Purchased/Referred Care (PRC) Training.”
[61] 42 CFR § 136.24 (2024).
[62] Julia Ysaguirre, “2025 Indian Health Service Purchased/Referred Care (PRC) Training.”
[63] Ibid.
[64] 42 CFR § 136, Subpart D and Subpart I (2024).
[65] Blue Cross and Blue Shield of New Mexico (BCBSNM), “IHS/PRC Fiscal Intermediary,” November 12, 2018, https://www.bcbsnm.com/ihsfi/pdf/ihs-tribal-services-brochure.pdf.
[66] Ibid.
[67] Indian Health Care Improvement Act, 25 U.S.C. § 1621(s).
[68] Prompt Payment Act, 31 U.S.C. § 3901.
[69] 42 CFR § 136.25 (2024).
[70] Indian Health Service, “Indian Health Manual - Services to Indians and Other - Chapter 3 Purchased/Referred Care Revisions.”
[71] 42 CFR § 136.25 (2024).
[72] Office of Inspector General, U.S. Department of Health and Human Services, Most Indian Health Service Purchased/Referred Care Program Claims Were Not Reviewed, Approved, and Paid in Accordance With Federal Requirements, A-03-16-03002 (2020), https://oig.hhs.gov/reports/all/2020/most-indian-health-service-purchasedreferred-care-program-claims-were-not-reviewed-approved-and-paid-in-accordance-with-federal-requirements/.
[73] Ibid.
[74] Ibid.
[75] Ibid.
[76] Ibid; Indian Health Service, Indian Health Manual, pt. 2, ch. 3, “Purchased/Referred Care,” sec. 2-3.21, “Prompt Action on Payment of Claims (PRC ‘Five-Day Rule’),” https://www.ihs.gov/ihm/pc/part-2/chapter-3-purchased-referred-care/#2-3.21.
[77] U.S. Government Accountability Office, Indian Health Service: Increased Oversight Needed to Ensure Accuracy of Data Used for Estimating Contract Health Service Need | U.S. GAO, GAO-11-767 (2011), https://www.gao.gov/products/gao-11-767.
[78] Ibid.
[79] Indian Health Service, Indian Health Care Improvement Fund (IHCIF) Workgroup Final Report (Rockville, MD: Indian Health Service, July 15, 2023), https://www.ihs.gov/sites/ihcif/themes/responsive2017/display_objects/documents/2023/IHCIFWorkgroupFinalReport.pdf.
[80] Indian Health Service, Indian Health Manual, pt. 2, ch. 3, “Purchased/Referred Care,” sec. 2-3.19, “Deferred Services,” https://www.ihs.gov/ihm/pc/part-2/chapter-3-purchased-referred-care/#2-3.19.
[81] U.S. Government Accountability Office, Indian Health Service.
[82] Cindy Marchand, “Prepared Statement of the Honorable Cindy Marchand, Secretary, Confederated Tribes of the Colville Reservation, House Committee on Appropriations Subcommittee on Interior, Environment, and Related Agencies, Public Witness Hearing—Native Americans,” The Confederated Tribes of the Colville Reservation, May 7, 2024, https://www.congress.gov/118/meeting/house/116219/witnesses/HHRG-118-II24-Wstate-MarchandC-20230727-U1.pdf.
[83] Confederated Tribes of the Colville Reservation, “Prepared Statement of the Honorable Cindy Marchand, Secretary, Confederated Tribes of the Colville Reservation,” submitted to the House Committee on Natural Resources, Subcommittee on Indian and Insular Affairs, Legislative Hearing on the “Restoring Accountability in the Indian Health Service Act of 2023,” July 27, 2023, https://www.congress.gov/118/meeting/house/116219/witnesses/HHRG-118-II24-Wstate-MarchandC-20230727-U1.pdf.
[84] Google Maps, Portland Area IHS Office to Colville Reservation Headquarters, accessed November 26, 2025, https://maps.app.goo.gl/WvUYcpEmG988GbZp7.
[85] Marchand, “Prepared Statement of the Honorable Cindy Marchand, Secretary, Confederated Tribes of the Colville Reservation, House Committee on Appropriations Subcommittee on Interior, Environment, and Related Agencies, Public Witness Hearing—Native Americans.”
[86] Ibid. Carryover refers to funds that remain on the Area’s books at fiscal year-end.
[87] Ibid. Notably, the remaining carryover (the difference between $33 million and $24 million) would encompass other Area PRC balances—such as open items associated with other Service Units or programs—and does not necessarily indicate that those funds were “meant for” Colville or any specific tribe. Further, a high carryover does not mean adequate funding existed to cover all outstanding PRC claims; rather, it may be attributed to factors like administrative backlog and delayed payment processing.
[88] Ibid.
[89] Purchased and Referred Care Improvement Act of 2024, H.R. 7516, U.S. Congress 118th Congress (2023–2024) (2045), https://www.congress.gov/bill/118th-congress/house-bill/7516/text.
[90] Purchased and Referred Care Improvement Act of 2025, H.R. 1418, U.S. Congress 119th Congress (2025–2026) (2025), https://www.congress.gov/119/bills/hr1418/BILLS-119hr1418ih.pdf.
[91] Ibid.
[92] Indian Health Service, “Director’s Workgroup on Improving PRC,” Purchased/Referred Care (PRC), https://www.ihs.gov/prc/director-s-workgroup-on-improving-prc/.
[93] Indian Health Service, “Director’s Workgroup on Improving PRC Membership,” March 28, 2025, https://www.ihs.gov/sites/prc/themes/responsive2017/display_objects/documents/prcri/directors_prc_workgroup.pdf.
[94] Ibid. IHS scheduling and meeting notices indicate that it has continued to meet regularly, including a meeting held in March 2025, suggesting that the Workgroup remains active.
[95] Roslyn Tso and Rohit Chopra, “CFPB and IHS Joint Letter Re: Protecting Approved Purchased/Referred Care Program Patients from Improper Bills,” December 12, 2024, https://www.consumerfinance.gov/about-us/newsroom/cfpb-and-ihs-joint-letter-re-protecting-approved-purchase-dreferred-care-program-patients-from-improper-bills/.
[96] Indian Health Care Improvement Act, Pub. L. No. 94-437, 90 Stat. 1400 (1976)(codified as amended at 25 U.S.C. §§ 1601 et seq.), https://uscode.house.gov/view.xhtml?req=granuleid:USC-prelim-title25-chapter18&num=0&edition=prelim; Fair Debt Collection Practices Act, Pub. L. No. 95-109, 91 Stat. 874 (1977) (codified as amended at 15 U.S.C. §§ 1692 et seq.), https://uscode.house.gov/view.xhtml?req=granuleid:USC-prelim-title15-chapter41-subchapter5&num=0&edition=prelim; and Fair Credit Reporting Act, Pub. L. No. 91-508, tit. VI, 84 Stat. 1114, 1127 (1970) (codified as amended at 15 U.S.C. §§ 1681 et seq.), https://uscode.house.gov/view.xhtml?req=granuleid:USC-prelim-title15-chapter41-subchapter3&num=0&edition=prelim.
[97] Consumer Financial Protection Bureau, Medical Collections on Credit Reports in Native American Communities, December 2024, 5–6, https://files.consumerfinance.gov/f/documents/cfpb_aian-medical-debt_2024-12.pdf. Note: In this report, CFPB defines “Native communities” and “majority-Native tracts” as census tracts where 50 percent or more of residents identify as American Indian or Alaska Native, alone or in combination with other races, in the American Community Survey.
[98] Sarah Liese, “Oklahoma Indigenous Cancer Rates Rising as Congress Spars over Future of IHS Funding,” Health, KOSU, July 30, 2025, https://www.kosu.org/health/2025-07-30/oklahoma-indigenous-cancer-rates-rising-as-congress-spars-over-future-of-ihs-funding.
[99] Stephanie C. Melkonian et al., “Incidence and Trends of the Leading Cancers with Elevated Incidence Among American Indian and Alaska Native Populations, 2012–2016,” American Journal of Epidemiology 190, no. 4 (2021): 528–38, https://doi.org/10.1093/aje/kwaa222. Note: In cancer surveillance, NH AI/AN refers to individuals recorded as American Indian/Alaska Native and not Hispanic in cancer registries or vital records (often supplemented by linkage with IHS patient files); this is a data category and does not necessarily indicate legal tribal citizenship. See CDC: Centers for Disease Control and Prevention, “Improving Cancer Data on American Indian and Alaska Native People,” National Program of Cancer Registries, January 14, 2025, https://www.cdc.gov/national-program-cancer-registries/about/american-indian-alaska-native-data.html.
[100] American Cancer Society, Cancer Facts & Figures 2022 - Special Section: Cancer in the American Indian and Alaska Native Population.
[101] CDC: Centers for Disease Control and Prevention, “Cancer in American Indian and Alaska Native People,” Cancer, January 29, 2025, https://www.cdc.gov/cancer/research/cancer-in-american-indian-and-alaska-native-people.html.
[102] CDC: Centers for Disease Control and Prevention, “Cancer and American Indian and Alaska Native People,” Cancer, May 7, 2025, https://www.cdc.gov/cancer/health-equity/american-indian-alaska-native.html.
[103] Oklahoma State Department of Health, 2024 Cancer Burden in the State of Oklahoma (2024), https://oklahoma.gov/content/dam/ok/en/health/health2/aem-documents/health-promotion/occr/Cancer%20Burden%20Report%202024_FINAL.pdf.
[104] Ayesha B. Sambo et al., Cancer in Oklahoma Data Brief Series: Cancer among the American Indian Population in Oklahoma, Volume 2 Issue 3 (Community Outreach and Engagement, Stephenson Cancer Center, OU Health, 2022), https://www.ouhealth.com/documents/Cancer-among-American-Indians-in-Oklahoma.pdf.
[105] United States Census Bureau, “A Look at the Largest American Indian and Alaska Native Tribes and Villages in the Nation, Tribal Areas and States,” Census.Gov, October 3, 2023, https://www.census.gov/library/stories/2023/10/2020-census-dhc-a-aian-population.html.
[106] Ibid.
[107] Sambo et al., Cancer in Oklahoma Data Brief Series: Cancer among the American Indian Population in Oklahoma.
[108] Ibid. In this instance, age adjustment standardizes rates to a common age distribution so that groups with different age structures can be compared.
[109] Ibid.
[110] Ibid.
[111] Melissa A. Jim et al., “Racial Misclassification of American Indians and Alaska Natives by Indian Health Service Contract Health Service Delivery Area,” American Journal of Public Health 104 Suppl 3, no. Suppl 3 (2014): S295-302, https://doi.org/10.2105/AJPH.2014.301933.
[112] Ibid.
[113] Ibid.
[114] CDC: Centers for Disease Control and Prevention, “Improving Cancer Data on American Indian and Alaska Native People.”
[115] David K. Espey et al., “Methods for Improving the Quality and Completeness of Mortality Data for American Indians and Alaska Natives,” American Journal of Public Health 104, no. Suppl 3 (2014): S286–94, https://doi.org/10.2105/AJPH.2013.301716.
[116] U.S. Department of Health and Human Services, Centers for Disease Control and Prevention and National Cancer Institute, “U.S. Cancer Statistics Working Group - U.S. Cancer Statistics Data Visualizations Tool - American Indian and Alaska Native, Non-Hispanic, United States, 2018-2022,” June 2025, https://www.cdc.gov/cancer/dataviz. For more information on the Centers for Disease Control and Prevention’s National Program of Cancer Registries, see [https://www.cdc.gov/national-program-cancer-registries/about/index.html]. For more information on the National Cancer Institute’s Surveillance, Epidemiology, and End Results Program, see [https://seer.cancer.gov/about/].
[117] U.S. Department of Health and Human Services, Centers for Disease Control and Prevention and National Cancer Institute, “U.S. Cancer Statistics Working Group - U.S. Cancer Statistics Data Visualizations Tool - American Indian and Alaska Native, Non-Hispanic, United States, 2018-2022.”
[118] Desi Small-Rodriguez and Randall Akee, “Identifying Disparities in Health Outcomes and Mortality for American Indian and Alaska Native Populations Using Tribally Disaggregated Vital Statistics and Health Survey Data,” American Journal of Public Health 111, no. S2 (2021): S126–32, https://doi.org/10.2105/AJPH.2021.306427.
[119] CDC: Centers for Disease Control and Prevention, “Cancer and American Indian and Alaska Native People.”
[120] U.S. Department of Health and Human Services Office of Minority Health, “American Indian and Alaska Native Health.”
[121] Ibid.
[122] Ibid.
[123] Ibid.
[124] Smita Bhatia et al., “Rural–Urban Disparities in Cancer Outcomes: Opportunities for Future Research,” JNCI Journal of the National Cancer Institute 114, no. 7 (2022): 940–52, https://doi.org/10.1093/jnci/djac030.
[125] Indian Health Service, INDIAN HEALTH SERVICE MEDICAL PRIORITY LEVELS.
[126] Ibid.
[127] Lani Hansen, “UKB Assumes Purchased and Referred (Contract Health) Program from IHS under Historic 638 Agreement,” United Keetoowah Band of Cherokee Indians in Oklahoma (UKB), August 26, 2024, https://www.ukb-nsn.gov/post/ukb-assumes-purchased-and-referred-contract-health-program-from-ihs-under-historic-638-agreement.
[128] Alaska Native Tribal Health Consortium, “ANTHC Fact Sheet: About Alaska Native Tribal Health Consortium,” June 2021, https://anthc.org/wp-content/uploads/2025/05/FY21-ANTHC-Fact-Sheet.pdf.
[129] Alaska Native Medical Center, “Alaska Tribal Health System Fact Sheet,” February 2023, https://www.ohsu.edu/sites/default/files/2023-08/ATHS%20ANTHC%20and%20ANMC%20fact%20sheets_updated%202023.pdf.
[130] Alaska Native Tribal Health Consortium, “ANTHC Fact Sheet: About Alaska Native Tribal Health Consortium.”
[131] “Native American Center of Cancer Health Excellence (NACCHE) > Home,” University of Oklahoma Stephenson Cancer Center, accessed November 26, 2025, https://nacche.ouhsc.edu/.
[132] Amanda E. Janitz et al., “Improving Care Coordination for Indigenous Patients with Cancer,” New England Journal of Medicine 393, no. 10 (2025): 940–42, https://doi.org/10.1056/NEJMp2506273.
[133] Fred Hutch Cancer Center, “Indigenous Cancer Health Excellence Initiative: Integrating Indigenous Values into Cancer Patient Advocacy and Research,” Fred Hutch, https://www.fredhutch.org/en/research/institutes-networks-ircs/ocoe/iche-i.html.
[134] Laurie Fronek, “Fred Hutch Receives Funding to Advance Indigenous Cancer Health Equity,” Fred Hutch Cancer Center, December 20, 2024, https://www.fredhutch.org/en/news/center-news/2024/12/funding-advance-indigenous-cancer-health-equity.html.
[135] American Cancer Society, “Honoring Indigenous Voices: Empowering Communities for a Healthier, Stronger Future,” Cancer.Org, https://www.cancer.org/about-us/what-we-do/multicultural/real-lives-indigenous-documentary.html.
[136] American Indian Cancer Foundation, “About American Indian Cancer Foundation,” American Indian Cancer Foundation, https://americanindiancancer.org/.
[137] CDC: Centers for Disease Control and Prevention, “Blue Beads Campaign Teaches American Indian Community About Colorectal Cancer,” National Comprehensive Cancer Control Program, May 7, 2025, https://www.cdc.gov/comprehensive-cancer-control/success-stories/blue-beads-campaign.html.
[138] Absentee Shawnee Tribal Health System, “Specialty Clinic,” Little Axe Health Center, https://www.asthealth.org/services/little-axe-health-center/specialty-clinic; Absentee Shawnee Tribal Health System, “Tariq Mahmood,” https://www.asthealth.org/providers/tariq-mahmood.
[139] Meredith L. Curtis and Valerie S. Eschiti, “Satellite Clinics for Cancer Care in Rural Communities,” Clinical Journal of Oncology Nursing 22, no. 5 (October 2018): 500–506, https://www.ons.org/pubs/article/23426/preview-download.
[140] Lance Madigan, “New Intermountain Health TeleOncology Partnership Brings Life-Saving Cancer Care to Interior Alaska,” Healthcare, PR Underground, August 19, 2025, https://www.prunderground.com/new-intermountain-health-teleoncology-partnership-brings-life-saving-cancer-care-to-interior-alaska/00359524/.
[141] See, for example, Arielle Zionts, Katheryn Houghton, “Patients Suffer When Indian Health Service Doesn’t Pay for Outside Care,” (Describing a Sisseton-Wahpeton Oyate tribal citizen living within the Standing Rock Sioux Tribe's PRCDA who sought PRC coverage for maternity care).
[142] Indian Health Service, Purchased/Referred Care (PRC) Process Diagram for Regular Patient / Provider Service.
[143] Fort Yates Hospital, “Fort Yates IHS Purchased Referred Care (PRC),” September 2020.
[144] Absentee Shawnee Tribal Health System, “Purchased Referred Care Guidelines,” October 2024, https://www.asthealth.org/sites/default/files/prc_2024_guidelines_-_final_edits-_11.6.24.pdf.
[145] Peter Christensen Health Center, “A Guide to Peter Christensen Health Center’s Purchased/Referred Care Services Program,” February 2022, www.pchclinic.com.
[146] Little Traverse Bay Bands of Odawa Indians (LTBB) Health Department, “Purchased/Referred Care (PRC),” LTBB Official Website, October 16, 2025, https://ltbbodawa-nsn.gov/departments/health-services/purchased-referred-care-prc/.
[147] Office of Inspector General, U.S. Department of Health and Human Services, Most Indian Health Service Purchased/Referred Care Program Claims Were Not Reviewed, Approved, and Paid in Accordance with Federal Requirements.
[148] Jacob Thayil et al., “How States and Tribes Can Leverage Medicaid to Improve the Health Care Delivered to American Indians and Alaskan Natives,” National Academy for State Health Policy, December 6, 2024, https://nashp.org/how-states-and-tribes-can-leverage-medicaid-to-improve-the-health-care-delivered-to-american-indians-and-alaskan-natives/.
[149] Absentee Shawnee Tribal Health, “American Rescue Plan,” Text, Absentee Shawnee Tribe, 2021, https://www.astribe.com/american-rescue-plan.
[150] Self-Governance Communication and Education Tribal Consortium (SGCETC), “Tribal Sponsorship Tool Kit,” Self-Governance Communication and Education Tribal Consortium (SGCETC), 2025, https://www.tribalselfgov.org/tribal-sponsorship-fast-track-key-tasks/.
[151] Allison Mitchell, Medicaid’s Federal Medical Assistance Percentage (FMAP), no. R43847 (Congressional Research Service (CRS), 2025), https://www.congress.gov/crs-product/R43847.
[152] For example, see Alicia Edwards, “Why Native Americans Should Have 3rd Party Health Coverage,” Great Plains Tribal Health Board News, May 26, 2022, https://www.greatplainstribalhealth.org/news/why-native-americans-should-have-3rd-party-health-coverage-148.html (highlighting how enrollment in Medicaid, Medicare, or private insurance can create new third-party revenue streams for local clinics).
[153] 42 U.S.C. ch. 7, subch. XVIII (2024); Paulette C. Morgan, Medicare Part B: Enrollment and Premiums, no. R40082 (Congressional Research Service (CRS), 2022), https://www.congress.gov/crs-product/R40082; Medicare eligibility and coverage requirements vary across Medicare Parts A–D; this report focuses on Medicare Part B premium assistance as an illustrative coverage strategy and does not describe Medicare Part A or other Medicare components in detail.
[154] Ibid.
[155] Oyate Health News, “At the Crossroads of Treaty and Policy: Tribal Leaders Sound the Alarm on Underfunding and Federal Cuts,” Oyate Health Center, March 2, 2025, https://www.oyatehealth.com/at-the-crossroads-of-treaty-and-policy-tribal-leaders-sound-the-alarm-on-underfunding-and-federal-cuts/.
[156] The National Tribal Budget Formulation Workgroup, The National Tribal Budget Formulation Workgroup’s Request for the Indian Health Service Fiscal Year 2026 Budget (2024), https://www.nihb.org/wp-content/uploads/2025/01/NIHB-FY26-Budget.pdf.
[157] Ibid.
[158] Indian Health Service, Justification of Estimates for Appropriations Committees, FY 2026, May 29, 2025, “FY 2026 President’s Budget,” 8, https://www.ihs.gov/sites/ofa/themes/responsive2017/display_objects/documents/FY_2026_IHS_Congressional_Justification_Plan.pdf.
[159] U.S. Congress, House Committee on Appropriations, Department of the Interior, Environment, and Related Agencies Appropriations Act, 2026, H.R. 4754, 119th Cong., 1st session, July 24, 2025, under “Department of Health and Human Services—Indian Health Service—Indian Health Services,” https://www.congress.gov/bill/119th-congress/house-bill/4754/text.
[160] Jordan Lofthouse, “Increasing Funding for the Indian Health Service to Improve Native American Health Outcomes,” Mercatus Center | George Mason University, January 31, 2022, https://www.mercatus.org/research/policy-briefs/increasing-funding-indian-health-service-improve-native-american-health.
[161] Mary Smith, “Native Americans: A Crisis in Health Equity,” American Bar Association, August 1, 2018, https://www.americanbar.org/groups/crsj/resources/human-rights/archive/native-americans-crisis-health-equity/.
[162] Indian Health Service, “Division of Budget Formulation,” Office of Finance and Accounting, https://www.ihs.gov/ofa/division-of-budget-formulation/.
[163] Elayne J. Heisler and Kate P. McClanahan, Advance Appropriations for the Indian Health Service: Issues and Options for Congress, no. R46265 (Congressional Research Service (CRS), 2020), https://crsreports.congress.gov.
[164] Erisel Cruz, “Federal Funding Lapses; Indian Health Service Remains Open for Business with Advance Appropriations,” National Indian Health Board, October 1, 2025, https://www.nihb.org/federal-funding-lapses-indian-health-service-remains-open-for-business-with-advance-appropriations/.
[165] National Indian Health Board, “National Indian Health Board | Advance Appropriations,” https://legacy.nihb.org/government-relations/advance_appropriations.php.
[166] Heisler and McClanahan, Advance Appropriations for the Indian Health Service: Issues and Options for Congress.
[167] U.S. Government Accountability Office, Indian Health Service: Agency Faces Ongoing Challenges Filling Provider Vacancies, GAO-18-580 (U.S. Government Accountability Office, 2018), https://www.gao.gov/assets/gao-18-580.pdf.
[168] Ibid.
[169] See, for example, Arielle Zionts, Katheryn Houghton, “Patients Suffer When Indian Health Service Doesn’t Pay for Outside Care,” (Describing a tribal citizen’s experience submitting an emergency care referral request, experiencing a long wait for approval, receiving no decision, and going into $1,500 debt).
[170] Indian Health Service, “Loan Repayment Program (LRP) Payment Examples,” Indian Health Service, https://www.ihs.gov/sites/loanrepayment/themes/responsive2017/display_objects/documents/LRP_Payment_Examples.pdf.
[171] U.S. Government Accountability Office, Indian Health Service: Agency Faces Ongoing Challenges Filling Provider Vacancies.
[172] Indian Health Service, “Indian Health Service Launches Largest Hiring Effort in Agency History,” Press Release, January 29, 2026, https://www.ihs.gov/newsroom/pressreleases/2026-press-releases/indian-health-service-launches-largest-hiring-effort-in-agency-history/; Clayton Fulton, “In Service to Our Relatives: IHS Announces Historic Hiring Initiative,” IHS Blog, January 29, 2026, https://www.ihs.gov/newsroom/ihs-blog/january-2026-blogs/in-service-to-our-relatives-ihs-announces-historic-hiring-initiative/.
[173] Arielle Zionts, Katheryn Houghton, “Patients Suffer When Indian Health Service Doesn’t Pay for Outside Care.”
[174] Indian Health Service, “Notice of Purchased/Referred Care Delivery Area Redesignation for the Pokagon Band of Potawatomi Indians of Michigan and Indiana,” Federal Register, November 22, 2024, https://www.federalregister.gov/documents/2024/11/22/2024-27457/notice-of-purchasedreferred-care-delivery-area-redesignation-for-the-pokagon-band-of-potawatomi.
[175] Ibid.
[176] Ibid.
[177] Veterans Affairs, “Community Care - Veteran Care Overview,” General Information, https://www.va.gov/COMMUNITYCARE/programs/veterans/index.asp; Givers, “Emergency Medicaid: What It Covers and How to Access | Givers,” Givers, January 10, 2025, https://www.joingivers.com/learn/emergency-medicaid.
[178] Indian Health Service, “Catastrophic Health Emergency Fund,” Federal Register, March 11, 2016, https://www.federalregister.gov/documents/2016/03/11/2016-05555/catastrophic-health-emergency-fund.
Notice of Use Statement: Copyright © 2026 - This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY-NC-NC 4.0). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
Disclaimer: This work has been created on behalf of the Native Nations Center for Tribal Policy Research (NNCTPR) which seeks to create high quality, non-partisan, neutral research related to Tribal Nations and their citizens. The NNCTPR endeavors to ensure the information presented is authoritative and accurate, but make no claims, promises, or guarantees about the completeness or adequacy of the content contained within this document. All claims expressed in this article do not necessarily represent those of the NNCTPR affiliated organizations, or those of the publisher, the editors and the reviewers.